-
Diet and Exercise as a PF Patient
Hello,
I am one of the columnist for PF News. I wanted to share my recent column about my experience with diet and exercise. I hope it is a help. Here is the link to the original column:
* * * * * * *
Trying to stay fit is extremely important for a PF patient. This is easier said than done. It is difficult to lose weight when you don’t move a lot, and it is hard to exercise when you feel tired and worn out all the time. I’ll bet you know what I mean.
I’ve had some recent success in both of these areas that I’d like to share with you. I’m motivated because I need to lose 37 pounds as one of the requirements for lung transplant consideration. I’ve lost 16 so far.
Eating
The transplant dietician at the University of California, San Francisco (UCSF) told me I could eat 1,000 calories a day as long as I got in 60 grams of protein, and ate lots of vegetables and fruit. I’ve been able to follow this plan, for which I am grateful. I record my weight and everything I eat on a free app for my phone called MyFitnessPal.I learned a lot once I started tracking what I was eating. Although I already ate fairly healthy at meals, I was eating lots of calories and snacking on carbs during the day. I’ve been able to substitute cut up vegetables, fruit, and protein bars when I get hungry.
Exercise
This is where I have made the most changes. I used to go to a pulmonary rehab gym two to three times a week. About a year ago, I had an exacerbation, which is an intensified sickness. Before this, I was using 6 liters per minute (lpm) of supplemental oxygen while sitting and 8 lpm while walking. After the exacerbation, I began using 8 lpm while sitting and 10 lpm while walking. Going to the rehab gym and exercising for 40 to 60 minutes really wore me out, and I couldn’t do much the rest of the day.When I told my doctor how much the rehab gym was wearing me out, he suggested that I exercise at home, in short amounts throughout the day. I’ve been doing this for three months, and it has helped to build stamina and increase my weight loss. I now exercise for 15 minutes three times a day, employing interval training. With this way of exercising, I work really hard, then rest, and repeat. You’ll see what I mean below. While exercising, I increase my oxygen to 10 lpm and wear an oximeter on my finger to monitor my heart rate and oxygen concentration. I have a list of exercises I pick from:

- Bicycle: I peddle as fast as I can until my O2 gets to 92 percent, then I rest until it gets back up to 97 percent. I repeat this cycle for 15 minutes.
- Walk in the house: I have a 25-foot cord for less restricted movement. I use this cord to quickly walk around my house until my O2 gets to 92 percent, then rest until it gets back up to 97 percent. I repeat this cycle for 15 minutes.
- Grocery shop or errands: I always wear an oximeter when I do errands to ensure my O2 levels and heart rate stay in the safe range. I have been told by my doctor not to go below 90 percent oxygen saturation or heart rate above 120 beats per minute (bpm).
- Weights: I’m pretty weak, so I use 1- or 2-pound weights to exercise my upper body. It is especially important to improve upper body strength because it helps us breathe better.
I try to spread out these short periods of exercise throughout the day. I’m losing weight more quickly, feeling better, and have decreased my need for oxygen to 6 lpm when sitting. Before my exercise program, I was using 8 lpm. I still need 10 lpm when walking.
It feels good to know that even though we have the deck stacked against us as PF patients, there are things we can do to increase our fitness level. Any progress is very meaningful. When I started this exercise program, I didn’t think I could do it. I did it anyway, though, and then started seeing some changes.
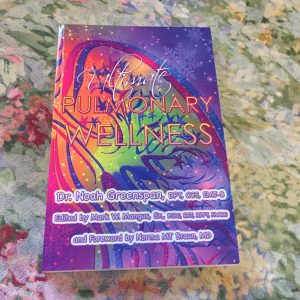
I’ve been inspired and helped so much by Dr. Noah Greenspan, a physical therapist and cardiovascular doctor. He’s also a pulmonary clinical specialist. He has dedicated his life to helping patients achieve the best pulmonary health possible. He wrote a book that I bought called “Ultimate Pulmonary Wellness.” I have really benefited from his work, as well as his website, which has a lot of wonderful information and videos. His book is available to read (but not download) online. Here is a link to his chapter on exercise. He also runs a Facebook group that I’m in. In it, he provides answers to patients’ questions, plus provides wonderful webinars about pulmonary health.
Please check with your doctor before employing any diet or exercise routines.
I hope this is a help to you.
Log in to reply.