Pulmonary Fibrosis Case Suggests PF Patients Should Be Screened For Autoimmune Diseases
Written by |
 A case study of pulmonary fibrosis (PF) in association with autoimmune diseases, entitled “A case of pulmonary fibrosis associated with rheumatoid arthritis, scleroderma sine scleroderma and ANCA associated vasculitis” was published in SpringerPlus by Dr. Amritpal Singh Anand from Lakeland Rheumatology and colleagues in Michigan describing a rare case of PF in association with rheumatoid arthritis (RA), scleroderma sine scleroderma (SSS) and anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV). The study led the researchers to highlight the importance of prognostic factors, histology, and radiographic features of the individual disease entities in the case study for the effective diagnosis, treatment, and prognosis of these overlapped diseases.
A case study of pulmonary fibrosis (PF) in association with autoimmune diseases, entitled “A case of pulmonary fibrosis associated with rheumatoid arthritis, scleroderma sine scleroderma and ANCA associated vasculitis” was published in SpringerPlus by Dr. Amritpal Singh Anand from Lakeland Rheumatology and colleagues in Michigan describing a rare case of PF in association with rheumatoid arthritis (RA), scleroderma sine scleroderma (SSS) and anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV). The study led the researchers to highlight the importance of prognostic factors, histology, and radiographic features of the individual disease entities in the case study for the effective diagnosis, treatment, and prognosis of these overlapped diseases.
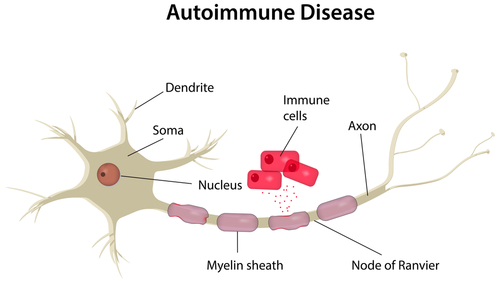
Diffuse parenchymal lung disease (DPLD) is a heterogeneous group of disorders characterized by inflammation and/or fibrosis of the parenchymal interstitium of the lung. Progression of disease results in impaired oxygen transfer and scarring within the lungs. The cause of DPLD can be unknown or due to other diseases, such as autoimmune diseases like as rheumatoid arthritis (RA), systemic sclerosis (SSc), dermatomyosits/polymyositis and anti neutrophil cytoplasmic antibody (ANCA) associated vasculitis.
[adrotate group=”3″]
It has been known that is PF is a common pathological consequence in a number of autoimmune diseases. In this new research, the authors describe a case study of a 71 year-old Caucasian woman with gradually worsening pulmonary fibrosis secondary to an overlap syndrome with rheumatoid arthritis (RA), scleroderma sine scleroderma (SSS), and anti neutrophil cytoplasmic antibody (ANCA) associated vasculitis (i.e. with more than one autoimmune condition), which makes her prognosis very poor. The researchers stressed that clinical prognosis depends on several factors like histology, baseline lung function, presence of auto-antibodies and their concentration and that prognosis status correlates negatively with the number of overlapped syndromes. Importantly, the authors emphasize the importance of identifying all the essential processes contributing to PF, mainly the diagnosis and confirmation of autoimmune diseases, and pointed out some of the parameters that should be included in the clinical evaluation.
Overall, the authors stated that patients with PF should be screened for autoimmune diseases, since the occurrence of overlap syndrome, where symptoms from two or more autoimmune conditions are identified in the same patient, may be possible. In addition, the clinical cases associated with more than one autoimmune syndromes need to be reported, due to the existence of very few studies. Importantly, the rapid and correct diagnosis and monitor of these individual autoimmune conditions will enable a better management and clinical outcome of these patients.