Stem Cells from IPF Patients Used to Create Working 3-D ‘Lungs’ to Aid in Research, Personalized Treatment
Written by |
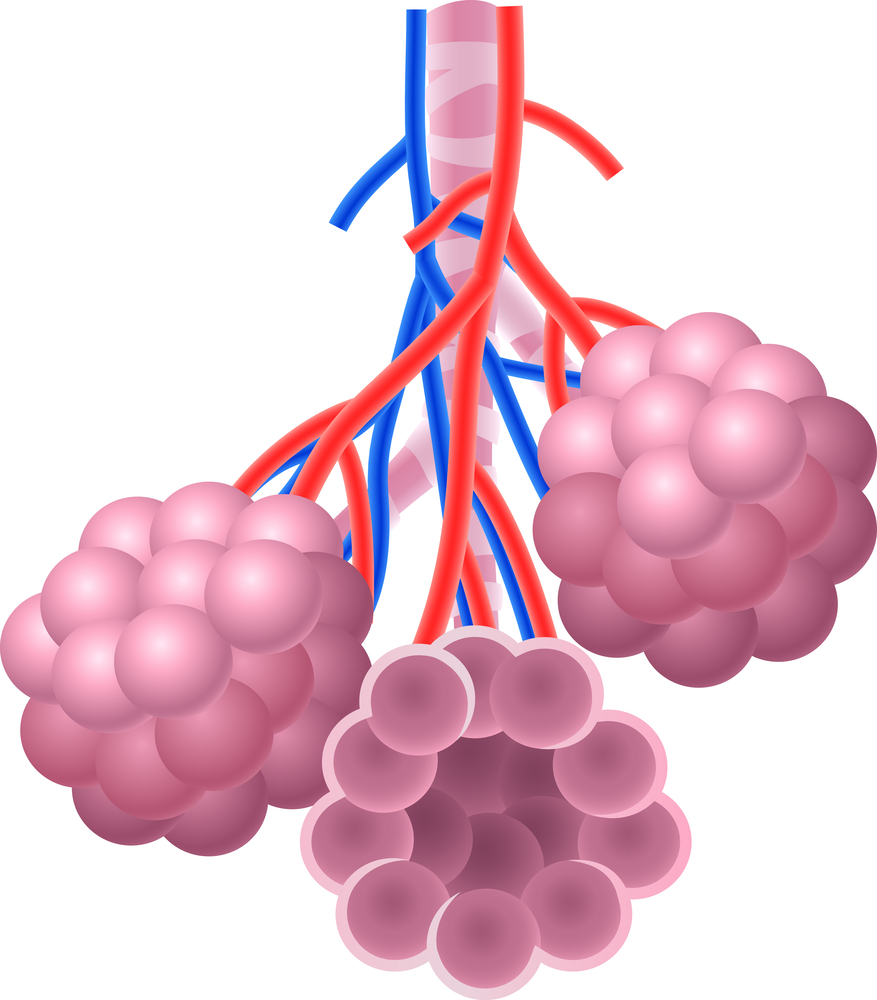
Researchers used stem cells from patients with idiopathic pulmonary fibrosis (IPF) to create a lung “organoid” — a three-dimensional structure similar to the human lung — that stands to improve studies into lung diseases like IPF and research into personalized drug therapies, by allowing such investigations to take place in an environment more closely resembling a real lung that is now possible with existing laboratory techniques.
The findings were published in the journal Stem Cells Translational Medicine, in the article “Development of a Three-Dimensional Bioengineering Technology to Generate Lung Tissue for Personalized Disease Modeling,”
“While we haven’t built a fully functional lung, we’ve been able to take lung cells and place them in the correct geometrical spacing and pattern to mimic a human lung,” Brigitte Gomperts, the lead author of the study by researchers at the University of California, Los Angeles (UCLA), said in a news release.
In past years, researchers have used ‘flat’ cultures of lung cells to study the role of genetic mutations or the effect of drug treatments. Although these cells originated from patients, in culture they looked healthy, making it difficult for scientists to study the pathology of the disease.
To address this problem, the team used stem cells — immature cells that can originate other cell types) — from IPF patients and allowed them to grow on top of sticky beads made of hydrogel, which were divided into small wells (7 mm each). In each well, the lung cells grew and established connections among themselves and around the beads, resulting in three-dimensional tiny structures that resemble the air sacs of the lungs. When certain molecular factors were added to these cultures, the “lungs” also developed scars similar to those observed in the IPF lungs, a finding that supported this technique providing a more realistic and reliable environment for future IPF studies.
“The technique is very simple,” said Dan Wilkinson, the study’s first author. “We can make thousands of reproducible pieces of tissue that resemble lung and contain patient-specific cells.”
Because several tiny organoids can be created at the same time using stem cells from each patient, this technique may also make it possible to test what drugs are effective for each person, allowing for the development of personalized medicine.