2 Distinct Groups of Lung Cells Seen to Play ‘Good’ and ‘Bad’ Roles in Diseases Like IPF
Scientists at the University of Pennsylvania identified two populations of lung mesenchymal cells that may play a distinct role such in diseases as pulmonary fibrosis — one that seems to protect against disease and the other possibly promoting it when things go awry.
Results suggest that future therapies targeting each cell type may boost lung regeneration while preventing the formation of fibrotic tissue.
The study, “Distinct Mesenchymal Lineages and Niches Promote Epithelial Self-Renewal and Myofibrogenesis in the Lung,” was published in the journal Cell.
The lung is a complex organ composed by a heterogeneous groups of cells, each with specialized roles. Some cells mediate the gas exchange by delivering oxygen to, and eliminating carbon dioxide from, the blood; others produce surfactant and mucous to lubricate the lungs, allowing for easy expansion and contraction; and still other cells are responsible for protecting the lungs from pathogens and pollution.
“The complicated structure of lungs is why it is difficult to quickly diagnose the exact type of lung disease a person may have with any certainty,” Edward E. Morrisey, a professor of cell and developmental biology, director of the Penn Center for Pulmonary Biology, and the study’s lead author, said in a press release.
“Also, as there is considerable reserve capacity in our lungs most people are not diagnosed with lung diseases such as IPF [idiopathic pulmonary fibrosis] until the disease has progressed significantly,” Morrisey added. Such delays mean that an IPF patient could lose a significant amount of lung function (up to 50%) before symptoms are evident.
The lungs’ complex cell profile suggests that different cells may contribute to disease-causing lesions, while other participate in the repair and regeneration mechanisms.
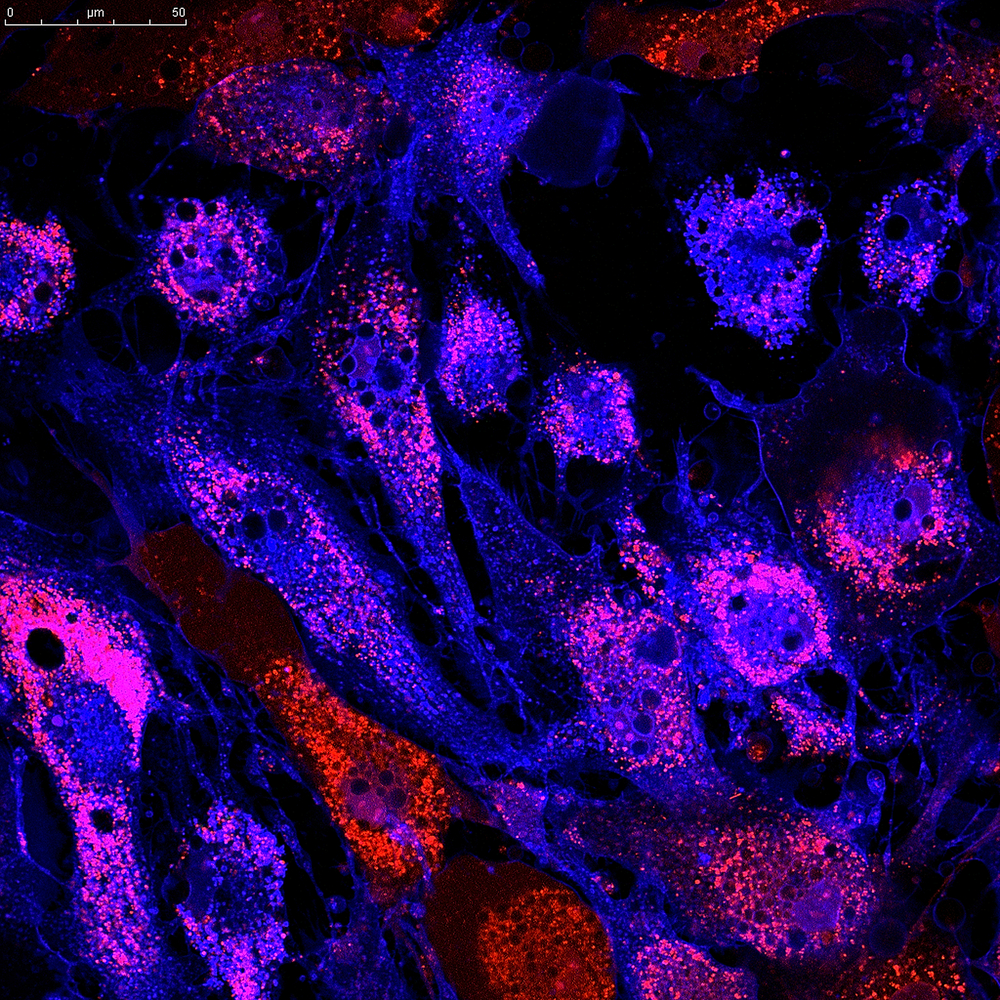
Researchers focused on lung mesenchymal cells, thought to play a role in maintaining lungs structure. The team studied gene expression in these cells at the single cell level. They found five distinct cell types, and performed further studies on two of them: the Mesenchymal Alveolar Niche Cell (MANC) and Axin2+ Myofibrogenic Progenitor cell (AMP).
MANC are vital for lung’s alveoli regeneration, while AMP were found to generate myofibroblasts, likely players in IPF development, as they generate scar tissue in response to injury. (Alveoli are the tiny air sacs in the lungs.)
Researchers analyzed the cells’ secretome — the collection of secreted molecules — and receptome — the receptors located at the cell’s surface — and compared findings to those from adjacent lung cells.
“One of the most important functions of these cells is to balance the repair and regeneration response after injury which occurs often due to the lung’s continual assault from the outside environment,” Morrisey said.
The analysis showed that MANCs are “good” cells as they promote self-renewal of gas-exchange cells, helping to maintain the alveoli during an adult’s life. Dysfunction or loss of MANCs is a likely event in lung diseases characterized by alveoli loss and diminished lung function, the study reports.
AMPs work to create scar tissue, but if such tissue growth is excessive and poorly controlled, these cells turn “bad” and become likely contributors to IPF, the researchers found.
The team’s next step is to identify these cells in the human lung. Morrissey and his team want to promote regeneration and reduce fibrotic response after injury by targeting MANCs and AMPs, and develop targeted therapies for lung diseases such as IPF.







