Extracellular Vesicles Likely Play Role in IPF Development, Study Reports
Tiny extracellular vesicles that carry information from one cell to another may contribute to the development of idiopathic pulmonary fibrosis (IPF) by carrying molecules involved in the disease, a study has found.
The study, “Increased Extracellular Vesicles Mediate WNT-5A Signaling in Idiopathic Pulmonary Fibrosis,” was published in the American Journal of Respiratory and Critical Care Medicine.
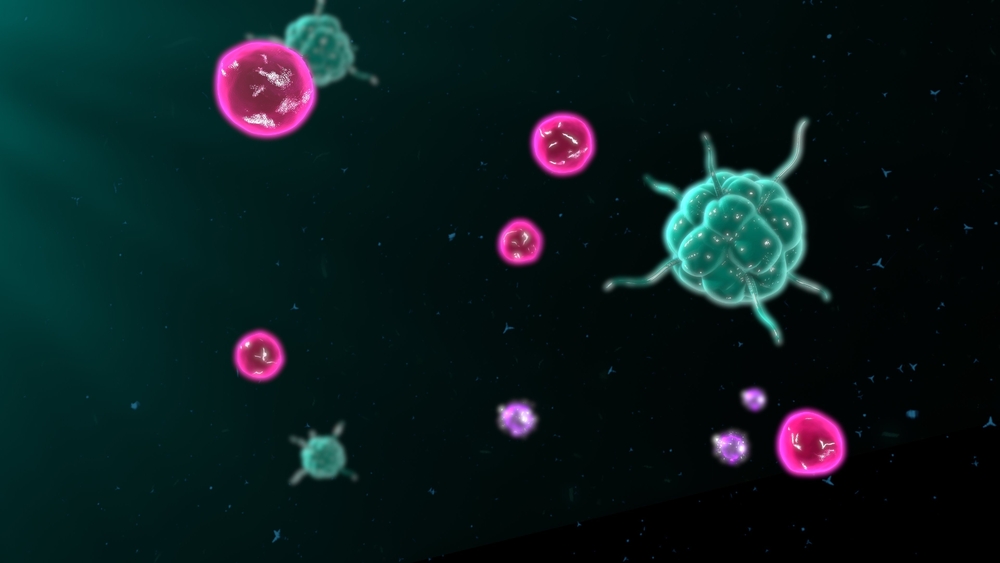
Scientists have only recently discovered that cells within our body can communicate with each other through vesicles that travel between them, known as extracellular vesicles. These can carry a multitude of molecules that elicit a specific effect in the target cells.
“Simply put, extracellular vesicles are tiny pouches released by cells that can contain a large number of messenger substances, such as proteins and nucleic acids,” Mareike Lehmann, one of the authors of the study, said in a press release. “They are an important means of communication between cells and organs and help to ensure that the substances reach completely new sites.”
Such communication plays important roles both in healthy and in disease conditions, including lung diseases. However, the particular role of extracellular vesicles in IPF was not clear.
So researchers in Germany conducted a study to shed light on how these vesicles might contribute to the development of IPF.
Join the PF forums: an online community for patients and caregivers living with Pulmonary Fibrosis.
Using samples from the bronchoalveolar lavage fluid, the researchers examined the presence and constitution of extracellular vesicles found not only in mice with lung fibrosis but also in IPF patients. The latter were compared with those of patients with interstitial lung disease other than IPF or healthy controls.
Mice with lung fibrosis and IPF patients had significantly more extracellular vesicles than the healthy controls. These vesicles carried a signaling molecule known as WNT5A, which had already been found to stimulate the proliferation of connective tissue cells and lead to fibrosis, or scarring.
Not surprisingly, when these vesicles were put on top of connective tissue cells, they induced their proliferation, suggesting that these vesicles play a key role in the development of IPF.
The effects were mediated by WNT5A, the researchers found. But blocking this signaling molecule with antibodies or disrupting the vesicles prevented the disease-causing effects.
“We were able to show in the study that increased levels of extracellular vesicles occur in IPF patients, which then act as carriers of WNT5A,” said lead author Aina Martin-Medina. “We were also able to confirm these results in our experimental model.”
“Characterization of [extracellular vesicle] secretion and composition may lead to novel approaches to diagnose and develop treatments for pulmonary fibrosis,” the researchers concluded.






