Mutation Prevents Mucus Clearance in Small Airways, Raising IPF Risk, Study Says
Written by |
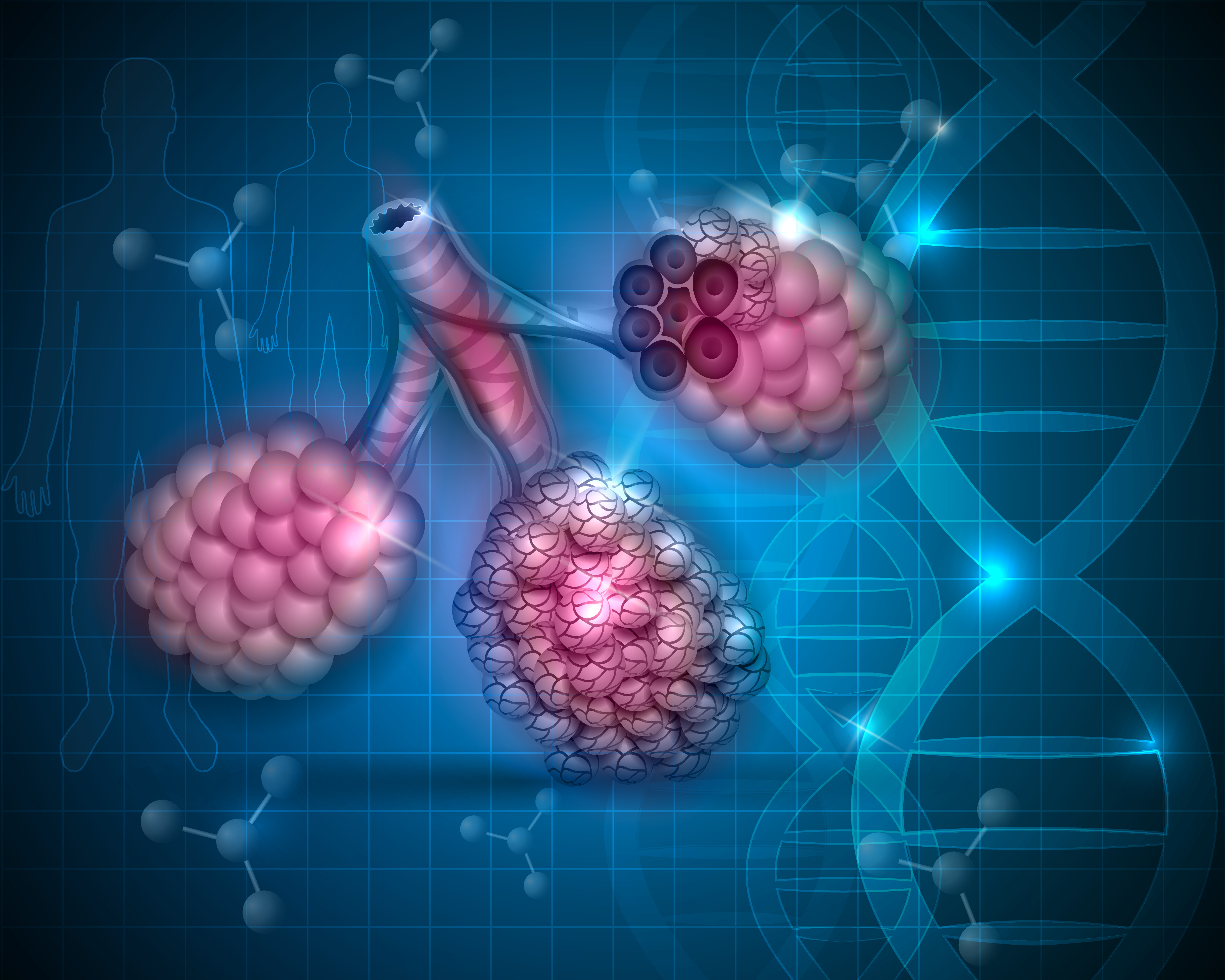
A study found a link between MUC5B-induced mucus accumulation and the progression of idiopathic pulmonary fibrosis, reporting that a MUC5B mutation can prevent mucus clearance in the small airways and induce scarring, indicating a strong risk factor in IPF.
The study, “Muc5b overexpression causes mucociliary dysfunction and enhances lung fibrosis in mice” was published in Nature Communications.
The MUC5B gene yields a protein member of the mucin family, which is a key component of mucus formation by giving mucus its gel-like features. Overexpression of the gene has been shown to be the strongest risk factor for IPF and for rheumatoid arthritis with interstitial lung disease.
Like for any gene, protein expression of MUC5B is controlled by a promoter, a stretch of DNA that initiates a process called gene transcription. Scientists at University of Colorado School of Medicine at CU Anschutz Medical Campus found that a mutation (rs35705950) in the MUC5B promoter increases the production of mucus in the small airways of the lungs.
This dysfunctional MUC5B gene results in mucus accumulation in the small airways, which can prevent proper lung (mucociliary) clearance, a primary and innate defense mechanism against pathogens.
The researchers say this mutated MUC5B promoter is a strong genetic risk factor for IPF.
Connect with other people and share tips on how to manage PF in our forums!
“The findings in this manuscript provide a critical breakthrough in understanding the cause and potentially the treatment of IPF by demonstrating that excess mucus in the small airways can cause lung fibrosis [scarring], in part, by impairing the mechanism of lung clearance,” David Schwartz, MD, chair of the department of medicine at CU School of Medicine, and the study’s senior author, said in a CU Anschutz news release written by Julia Milzer.
The researchers went on to suggest that targeting MUC5B in the small (distal) airways could be an effective approach to prevent the progression of pulmonary fibrosis.
“These discoveries have provided the means to identify an at-risk population, diagnose the disease prior to the development of irreversible scarring, focus on a unique therapeutic target (MUC5B) and a specific location in the lung (distal airway), and create a novel pathway for therapeutic intervention for a disease that is currently incurable,” Schwartz added.
Further in vivo experiments using a mucus dissolving agent in mouse models overexpressing MUC5B resulted in improved lung clearance and suppression of lung fibrosis.
“This study shows how genetic findings in human diseases can generate new hypotheses, such as those related to impaired mucociliary clearance, that may lead to the discovery of novel molecular mechanisms and the development of early diagnostics and more accurate treatments for pulmonary fibrosis,” said James P. Kiley, PhD, director of the division of lung diseases at the National Heart, Lung, and Blood Institute.





