Esbriet Treatment Seems Safe in IPF Patients With Lung Cancer, Study Reports
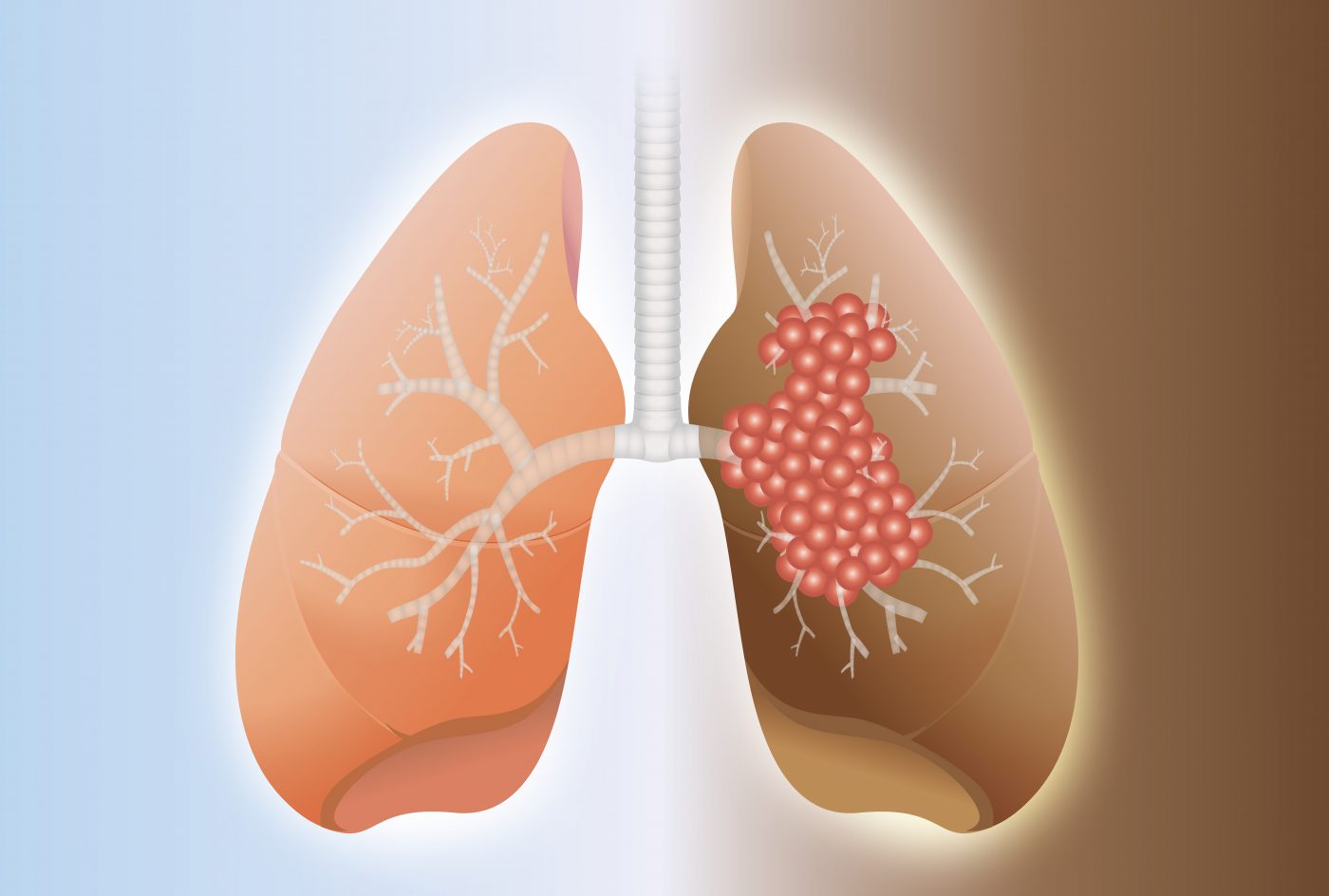
Esbriet (pirfenidone), an approved treatment for idiopathic pulmonary fibrosis (IPF), seems to be safe in IPF patients who also have non‐small cell lung cancer (NSCLC) when combined with cancer therapy.
The finding is detailed in the study, “Safety and effectiveness of pirfenidone combined with carboplatin‐based chemotherapy in patients with idiopathic pulmonary fibrosis and non‐small cell lung cancer: A retrospective cohort study,” published in the journal Thoracic Cancer.
A high incidence of acute exacerbations (AE) — a sudden worsening of disease symptoms — has been reported in IPF patients treated with certain chemotherapy agents, such as Paraplatin (carboplatin).
Esbriet, marketed by Genentech, and Ofev (nintedanib), manufactured by Boehringer Ingelheim), are approved antifibrotic agents able to delay the progression of IPF. Both have also been reported to prevent AE.
However, no studies have investigated the preventive ability of these antifibrotic agents against AE induced by chemotherapy or immunotherapy in people with both IPF and NSCLC.
Thus, researchers in Japan conducted a study to assess the safety and effectiveness of Esbriet combined with two types of cancer treatment: carboplatin‐based chemotherapy or immunotherapy with immune checkpoint inhibitors (ICIs). ICIs are molecules that restore an anti-tumor immune response in the body.
In total, 14 patients with IPF and NSCLC were analyzed. The team assessed AE occurrence associated with treatment, as well as overall survival and progression‐free survival (PFS), or the time a person lives with a disease without it getting worse.
As first‐line chemotherapy, the patients were treated with Esbriet combined with Paraplatin and paclitaxel (available under several brand names) or Teysuno (S‐1; tegafur/gimeracil/oteracil). After disease progression was confirmed, these individuals received cytotoxic agents — agents toxic to cells — or ICIs, including Opdivo (nivolumab), by Bristol-Myers Squibb, and Keytruda (pembrolizumab), by Merck.
Regardless of cancer progression or chemotherapy changes, Esbriet treatment was maintained.
Most patients (10 out of 14) were classified as GAP stage I, the lowest level on the gender, age, and physiology (GAP) score, an index of disease severity.
The results showed that the median PFS was 110 days (about 3.6 months) for lung cancer and 447 days (about 15 months) for IPF. The median overall survival was 362 days (just less than one year) in patients with IPF and NSCLC.
This overall survival was relatively longer than that found in previous studies, the team noted, which led them to suggest that Esbriet might potentially extend the survival rate in these patients.
Additionally, Esbriet was used until the last late‐line chemotherapy administration.
“This suggests that patients with IPF and NSCLC can tolerate the combination of pirfenidone and carboplatin‐based chemotherapy,” the researchers wrote.
The incidence of AE in the patient group analyzed was 18% in one year of combined treatments.
“The cumulative incidence of AE‐IPF [acute exacerbation of IPF] … was lower than that presented in an earlier report investigating patients with IPF and NSCLC who did not receive pirfenidone,” researchers wrote.
Importantly, the team found that none of the patients developed AE associated with first‐line chemotherapy, specifically Esbriet combined with Paraplatin and paclitaxel or Teysuno. Further, regarding patients who received ICIs (four patients), none of them developed ICI‐related AE.
“No patients with IPF and NSCLC who received pirfenidone in combination with first‐line carboplatin‐based chemotherapy or late‐line ICIs developed acute IPF exacerbations,” the researchers wrote.
Overall, the findings suggested that Esbriet “might have a prophylactic effect against chemotherapy‐associated AE‐IPF,” and that Esbriet “combined with carboplatin‐based regimens or ICIs might be safe first‐line chemotherapy for patients with IPF and NSCLC,” the team wrote.
Further studies are needed, however, to assess “the safety and effectiveness of combined chemotherapy using antifibrotic agents and ICIs” the researchers noted.






