Idiopathic Pulmonary Fibrosis Disease Worsening Can Be Predicted by Measuring Lung Inflammation, According to Study
A recent scientific article from researchers in Italy proposes that innate immune responses specific to individual patients could determine how rapidly idiopathic pulmonary fibrosis (IPF) progresses. The research study, titled “Immune Inflammation and Disease Progression in Idiopathic Pulmonary Fibrosis“ appeared May 9, 2016 in the journal PLoS One.
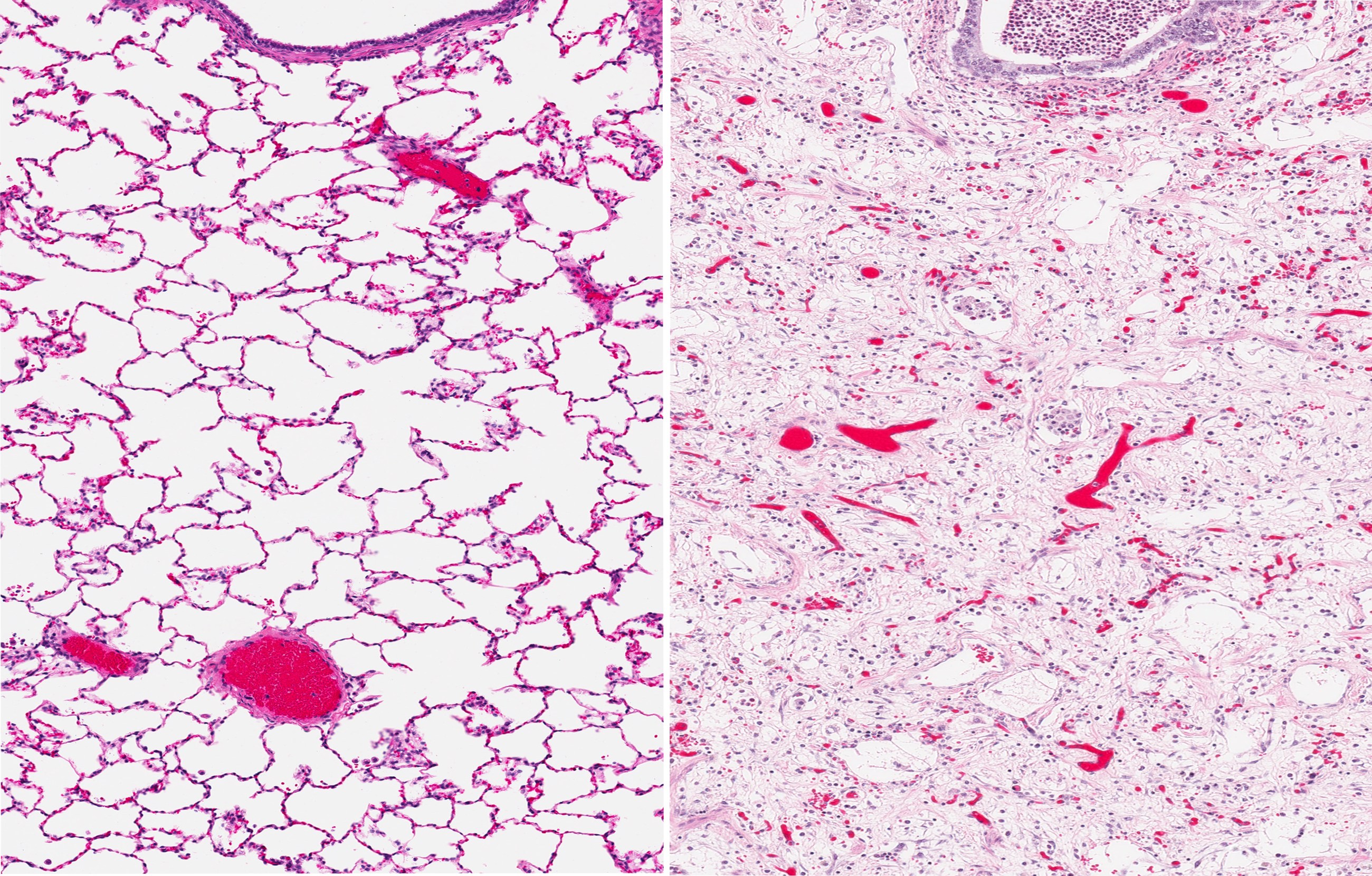
IPF refers to the thickening and scarring (referred to as fibrosis) of lung tissue, which results in difficulty breathing and is eventually fatal. The clinical course of IPF makes treatment complicated, since some patients experience rapid deterioration, while the disease progresses slowly in the majority of individuals with IPF. It is currently difficult to predict how IPF will affect an individual patient.
The research team led by Elisabetta Balestro of the Department of Cardiac, Thoracic and Vascular Sciences, University of Padova, Italy wanted to know which individual characteristics could determine how rapidly IPF progresses. To understand this, the team studied clinical and functional data taken from 73 IPF patients, who were potential lung transplant candidates. They measured forced vital capacity (FVC), and how much it changed in a year to see how rapidly IPF symptoms increased. FVC is an assessment of how much air a person can force out of the lungs and is a standard IPF clinical test. The scientists also looked for abnormalities in the lungs in 41 patients who eventually did have a lung transplant.
The researchers found that at diagnosis, there were 48 individuals with slow disease progression, based on the FVC test, and 25 individuals with rapid IPF progression. A total of 11 slow and 3 rapid progressors had an acute exacerbation during the study. An acute exacerbation is a sudden worsening of lung symptoms.
Rapid progressors had more lung inflammation than slow progressors, meaning that they had a greater number of immune system cells and molecules produced by those cells. Those who experienced an acute exacerbation also had more lung inflammation compared with those who did not have an acute exacerbation. Lung inflammation correlated with the decline in the volume of air expelled during the FVC test.
In their published study report, the investigators concluded that “an innate and adaptive inflammation appears to be a prominent feature in the lung of patients with IPF and could contribute to determining of the rate of disease progression.”
Overall, the study indicated that measurements of lung inflammation, including immune cells and inflammatory molecules, could help to predict how quickly people with IPF will have an increase in disease symptoms and decline in lung function. This could help physicians predict how IPF will affect an individual patient, and may eventually aid in the selection of IPF treatments.







