New Study Outlines Biological Mechanisms in Idiopathic Pulmonary Fibrosis
Written by |
 A study published this week in The Journal of Molecular Medicine Reports discussed the discovery of biological mechanisms that may have important implications in the future treatment of idiopathic pulmonary fibrosis (IPF). The research was conducted by an international team of collaborating scientists from the University Putra Malaysia, Michigan State University, and University Malaysia Sabah. This study utilized a mouse model in the laboratory to test a possible connection between a component of the body’s immune system and the cause of IPF.
A study published this week in The Journal of Molecular Medicine Reports discussed the discovery of biological mechanisms that may have important implications in the future treatment of idiopathic pulmonary fibrosis (IPF). The research was conducted by an international team of collaborating scientists from the University Putra Malaysia, Michigan State University, and University Malaysia Sabah. This study utilized a mouse model in the laboratory to test a possible connection between a component of the body’s immune system and the cause of IPF.
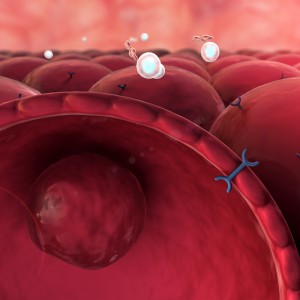
IPF is a chronic disease that results in a scarring and thickening of lung tissue, without a known cause. It is considered an orphan disease, meaning that it is extremely rare and its precise incidence and prevalence rates globally are unknown. Studies have shown that these rates of IPF are increasing globally, and may not be considered rare in the near future. The unknown origin of the disease has led to speculation among scientists that it may be environmentally linked, in which case the lungs are responding to injury such as chronic cigarette smoking or exposure to chemicals. Genetic and immune dysfunction has also been thought to possibly play a role in disease manifestation.
[adrotate group=”3″]
This study was designed to investigate a cytokine protein component of the immune system known as Transforming growth factor-β (TGF-β). Cytokine proteins have important cell signaling/communication functions required for healthy immune system response to disease. TGF-β’s role is specifically related to the inflammatory response which when unregulated, can cause an autoimmune (triggered by a body’s own immune system) reaction in lung tissue, such as inflammation and scarring. This role in immune response led researchers to question TGF- β’s significance in the cause of IPF. The experiments conducted in this study used an inhibitor of the TGF-β protein, SB 431542, to ascertain if the cytokine did play a role in pathogenesis of IPF disease.
The results of this animal study suggested that the inhibition of TGF-β function by SB 431542 may reduce the clinical disease pathology associated with pulmonary fibrosis. Future studies will need to be completed to further explore the possible connection between dysfunctional cytokines and the onset of IPF. This study adds to the body of knowledge that will one day shed light on the cause of IPF, and hopefully a cure.






