Pulmonary Fibrosis May Be Caused By Excess Fat in the Lungs
 Special cells may dump fat into the lungs of people with pulmonary fibrosis, filling airspaces. Scientists at Thomas Jefferson University in Philadelphia found that decreasing the accumulation of lung fat could help reduce problems associated with this disease.
Special cells may dump fat into the lungs of people with pulmonary fibrosis, filling airspaces. Scientists at Thomas Jefferson University in Philadelphia found that decreasing the accumulation of lung fat could help reduce problems associated with this disease.
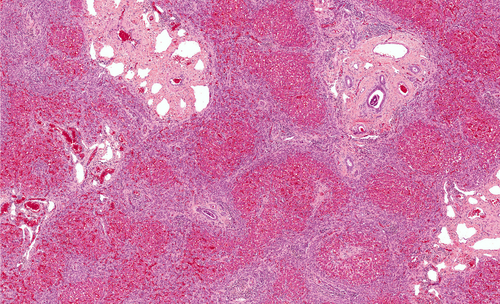
Pulmonary fibrosis is characterized by scarred, thick tissue within the lungs. This scarring is known as fibrosis, which causes difficulty with breathing. The condition has no cure, and patients typically live only three to five years following diagnosis, with lung transplant as the only current possible treatment.
People with pulmonary fibrosis have cells filled with excessive fat (lipids) within the lungs. These cells are known as “foam cells.” How foam cells contribute to pulmonary fibrosis is unknown.
The investigators, led by Ross Summer MD, Associate Professor in the department of Pulmonary and Critical Care Medicine at Thomas Jefferson University, examined a mouse model of lung fibrosis caused by a chemical called bleomycin. Bleomycin is known to cause pulmonary fibrosis and problems with lung functioning. Foam cells responded to the chemical by contributing excessive levels of fat within the lung airspaces. These levels of lipids exceeded the amount that is normally found in the lung. The fat accumulation also occurred prior to the formation of fibrosis, at around three days following bleomycin. Fibrosis began to form at approximately 14 days after the chemical was given, as measured by collagen, an indicator of scar tissue formation.
The scientists then tested whether foam cells and fat accumulation occur in response to other known inducers of lung fibrosis, silica exposure and radiation injury. With these two types of fibrosis-inducers they again observed that foam cells accumulate in the lungs, preceding the formation of fibrosis.
According to first author, Freddy Romero, PhD, “Both the initial damage to the cells lining the airway of the lung and the inflammation are important, but the thing that drives the damage is the unregulated excess lipids in the distal airspaces.”
[adrotate group=”3″]
The researchers used a substance called granulocyte macrophage colony-stimulating factor (GM-CSF) in mice treated with bleomycin, to reduce the secretion of lipids and to help promote lipid removal in the lungs. This protein is naturally secreted by cells known as macrophages. GM-CSF reduced lung fibrosis by over 50 percent, based on collagen levels.
According to Summer, “These results show, for the first time, that a break-down of normal lipid handling may be behind this lung disease. If we prove that the same process holds true in humans, it suggests that we could prevent or mitigate the disease by simply clearing out the excess oxidized lipids from lungs.”
With regard to future treatments, Summer noted that, “Currently, there are no drugs available to inhibit foam cell formation but we are working on developing these treatments. We do not believe inhibiting lipid synthesis would be a good idea since lipids are needed for generating the surfactant material that normally baths the respiratory epithelium. Instead, we believe that therapies which block foam cell formation or promote the release of lipids from foamy macrophages might be more effective.”
The study was published in the November 19th issue of the American Journal of Respiratory and Critical Care Medicine.







