Statins Do Not Contribute to IPF Worsening, Analysis of Ofev Trial Data Shows
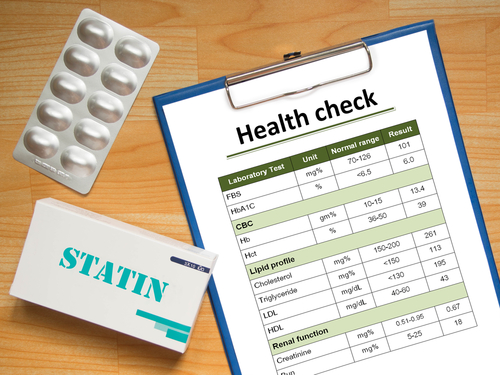
Using statins to prevent cardiovascular disease is safe for idiopathic pulmonary fibrosis patients, according to an analysis of trial data on the IPF therapy Ofev (nintedanib).
Statin therapy does not contribute to lung function decline or diminish Ofev’s effectiveness in IPF patients, researchers said. Their analysis of data from the INPULSIS trials appeared in the journal Respiration.
It is known that IPF increases the risk of heart diseases. So, it is common for IPF patients to receive medications aimed at reducing cardiovascular risk, including statins, which lower cholesterol levels.
Statins also have anti-inflammatory and anti-oxidant properties, and non-clinical-trial studies have shown that they can inhibit key molecules involved fibrosis. In contrast, other studies have suggested that statins contribute to the progression of idiopathic lung disease.
In the study, “Statin Therapy and Outcomes in Trials of Nintedanib in Idiopathic Pulmonary Fibrosis,” an international research team evaluated statins’ impact on IPF patients’ outcomes.
The analysis was based on data collected from the two Phase 3 INPULSIS trials (NCT01335464 and NCT01335477). A total of 312 patients were receiving statins at baseline while 749 were not. All participants were randomized to receive 150 mg of Ofev, which is marketed by Boehringer Ingelheim, or a placebo twice a day for 52 weeks.
Evaluation of lung function showed that patients receiving statin therapy and Ofev had less decline in pulmonary capacity, compared with a placebo. The yardstick that researchers used was patients’ annual rate of decline in forced vital capacity (FVC). The results suggested that statins do not diminish Ofev’s effectiveness.
The team also analyzed if statins could alter the progression of IPF. In the group of patients treated with a placebo, statins did not change outcomes, with similar time to FVC decline. In addition, statins did not trigger any change in time to first acute exacerbation.
“Taken together, these data suggest that statins do not have a negative influence in patients with IPF, and there is no evidence to suggest that these drugs need to be discontinued,” the researchers wrote.
“It remains unclear whether statin therapy has a positive effect on the clinical course of IPF; this could only be determined through a prospective randomized controlled trial,” the team concluded.







