Acute Exacerbation of Idiopathic Pulmonary Fibrosis Caused by Macrophage Activation
 In a recent study entitled “Macrophage Activation in Acute Exacerbation of Idiopathic Pulmonary Fibrosis,” a team of researchers show acute exacerbations in idiopathic pulmonary fibrosis are caused by multifactorial cellular responses, including macrophage activation. The study was published in the open access journal Plos One.
In a recent study entitled “Macrophage Activation in Acute Exacerbation of Idiopathic Pulmonary Fibrosis,” a team of researchers show acute exacerbations in idiopathic pulmonary fibrosis are caused by multifactorial cellular responses, including macrophage activation. The study was published in the open access journal Plos One.
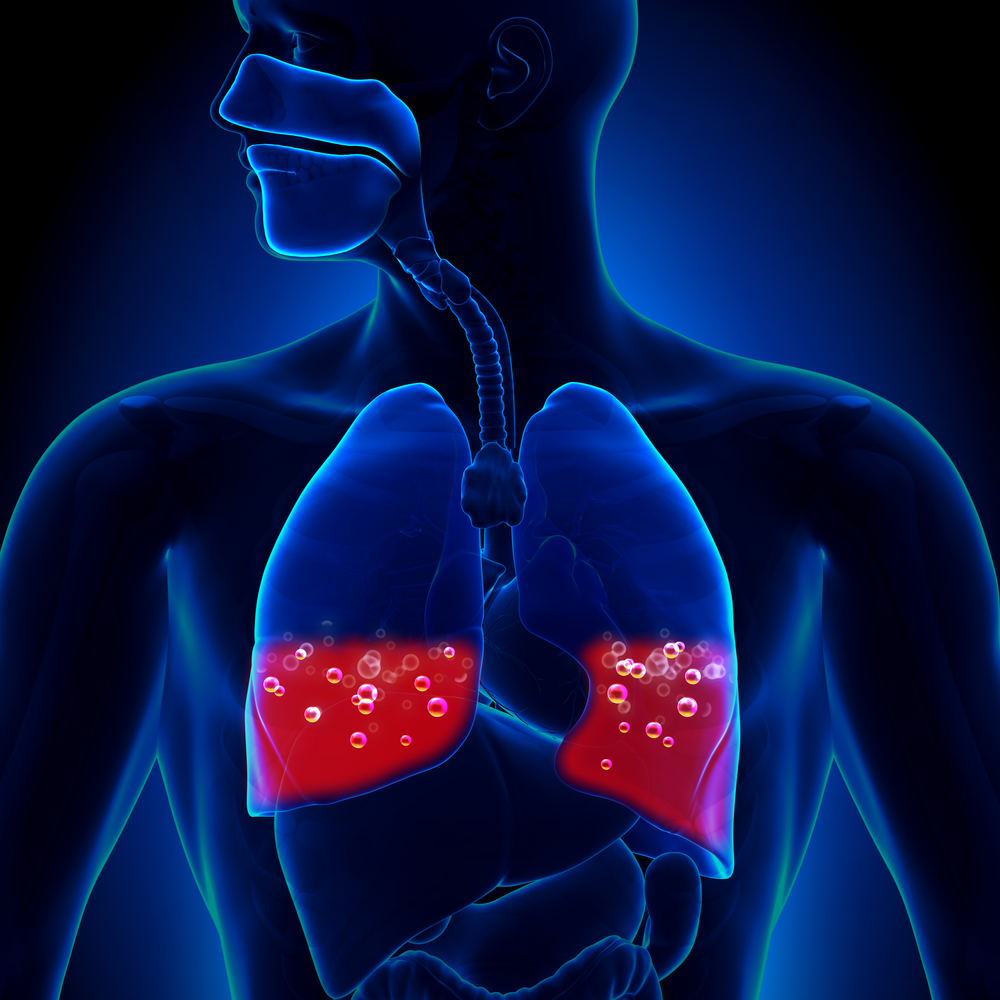
Idiopathic pulmonary fibrosis (IPF) is a chronic lung disease characterized by severe damage to the alveoli (the air sacs of the lungs) and lung tissue that, with time, becomes thick and scarred. This thickening of lung lining tissue results in an irreversible loss of the lungs’ ability to transport oxygen. Therefore, IPF is a fatal disease, ultimately culminating in patients’ death most frequently by respiratory failure, but also due to pulmonary hypertension, heart failure, pulmonary embolism, pneumonia and lung cancer. The disease progresses from mild symptoms to acute exacerbations, characterized by an accelerating decrease of respiratory function and lung damage, which were previously recognized as major factors for patients’ death. However, the mechanisms leading to acute exacerbations remain poorly understood, with two ideas currently in debate: one suggesting that acute exacerbations are mainly a random event caused by external factors, while the second suggests it is caused by intrinsic cellular mechanisms.
[adrotate group=”4″]
A team of researchers at the Department of Pneumology, University Medical Centre, Freiburg, Germany tackled this issue to determine whether cellular mechanisms, and which of those, were underlying acute exacerbations in IPF disease. They hypothesized that, as fibrotic lung diseases (IPF is also included in this group) exhibit activation of a specific type of macrophages (important cells of the immune system) — the M2 macrophages — they studied macrophage activation in IPF patients with acute exacerbations. The authors performed to 71 therapy-naive patients with IPF a standardized bronchoscopy with bronchoalveolar lavage (BAL) — a minimally invasive procedure to collect a lung sample for evaluation. They observed that IPF patients with acute exacerbations had an increased profile of immune cells and cytokines, in agreement with the profile seen with acute lung injury and wound healing processes. Specifically, they observed an increase in neutrophils and M2 macrophages in BAL samples of IPF patients with acute exacerbations, with M2 macrophages showing an increase in cytokine production. Notably, the authors found that CCL18 cytokine production was a marker for a future development of acute exacerbations.
Thus, the authors highlight that their findings suggest that acute exacerbations in IPF patients are indeed caused by activation of cellular mechanisms, such as M2 activation, and are not due to external factors alone. The authors finally suggest that a future therapeutic to prevent acute exacerbations may therefore target macrophage activation.







