Researchers Discover Mechanism Underlying Acute Lung Injury and Pulmonary Fibrosis in Paraquat Poisoning

 Researchers from Shanghai Jiao Tong University in China published in the journal BioMed Research International their findings on the mechanism behind acute lung injury and pulmonary fibrosis observed after poisoning with the chemical paraquat. The study is entitled “DNaseI Protects against Paraquat-Induced Acute Lung Injury and Pulmonary Fibrosis Mediated by Mitochondrial DNA.”
Researchers from Shanghai Jiao Tong University in China published in the journal BioMed Research International their findings on the mechanism behind acute lung injury and pulmonary fibrosis observed after poisoning with the chemical paraquat. The study is entitled “DNaseI Protects against Paraquat-Induced Acute Lung Injury and Pulmonary Fibrosis Mediated by Mitochondrial DNA.”
Acute lung injury (ALI) is a common condition characterized by acute severe hypoxia (low oxygen levels), pulmonary edema and dysfunction at the respiratory level. This condition is thought to be triggered by local or systemic inflammation. Pulmonary fibrosis (PF) can result from ALI; it is also a severe and progressive disease that affects the lungs, causing a permanent loss of lung tissue and impairment in oxygen transfer. Both lung diseases have extremely high morbidity and mortality.
Poisoning with the highly toxic paraquat (PQ) compound (an herbicide) can cause ALI and irreversible PF in both humans and animals. There is no antidote or effective treatment for this chemical. PQ poisoning can be used as a unique disease model for both ALI and PF, although the mechanism underlying its effects on lung function are unknown.
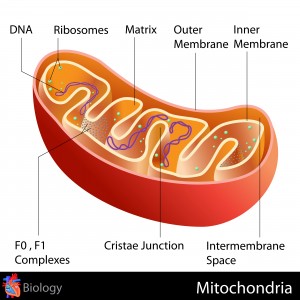
PQ has been suggested to target the cellular organelle mitochondria (known as the powerhouses of the cell, which generate energy for the body). Researchers therefore studied in more detail the possible effect of PQ poisoning in mitochondria and how it leads to lung injury.
[adrotate group=”3″]
The team found that PQ is indeed able to injure the mitochondria, which results in the release of mitochondrial DNA (mtDNA). Since mtDNA contains specific modifications that resemble the ones present in bacterial DNA, once mtDNA is released into the cytoplasm of the cells, it can trigger the innate immune system that causes a systemic inflammatory response. As part of this immune response, researchers found that peripheral blood mononuclear immune cells (PBMCs) are recruited, and that alveolar epithelial cells are stimulated to produce TGF-β1 (a key profibrotic molecule). Interestingly, it was found in vitro that it was possible to reverse the effects of mtDNA in the presence of DNase I, a nuclease able to cut and fragment DNA molecules.
Using PQ-induced lung injury rodent models, the team found that the levels of circulating mtDNA and bronchial alveolar lavage fluid were higher. Remarkably, in line with the in vitro results, an intravenous administration of DNase I resulted in the protection of the lungs from the effects of PQ, significantly improving animal survival. Furthermore, as mtDNA was eliminated by DNase I, the expression of known ALI biomarkers (such as TNFα, IL-1β, and IL-6) was downregulated. Researchers believe that the PQ-induced ALI and PF mechanism via mtDNA release is most likely also occurring in other types of induced lung injury.
The team concluded that DNase I elimination of released mtDNA can be used as a potential therapeutic approach and suggest that clinical trials should be performed to establish the potential of DNase I as a therapy for PQ-induced lung injury.







