Protective Mechanism in Lung Immune Cells, Mitophagy, Surprises by Contributing to PF Development
Mitophagy, a protective mechanism against mitochondria reactive oxygen species (ROS), in lung macrophages is a key mechanism underlying the development of pulmonary fibrosis, according to a study titled “Macrophage Akt1 Kinase-Mediated Mitophagy Modulates Apoptosis Resistance and Pulmonary Fibrosis,” and published in the journal Immunity.
Alveolar macrophages, immune cells located in the lungs, are key players in idiopathic pulmonary fibrosis (IPF) pathogenesis by triggering an immune response that leads to the production and secretion of a molecule called transforming growth factor beta, or TGF-β1, which is associated with damage to lung tissue.
A team of researchers at the University of Alabama, Birmingham (UAB), investigated further the pathways leading to TGF-β1 production. The team found that alveolar macrophages are the primary cells responsible for TGF-β1, and that its secretion is important for pulmonary fibrosis. Performing studies with alveolar macrophages from both a mouse model with bleomycin-induced lung injury and patients with IPF, researchers discovered that mitochondria ROS and mitophagy underlie increased expression of TGF-β1.
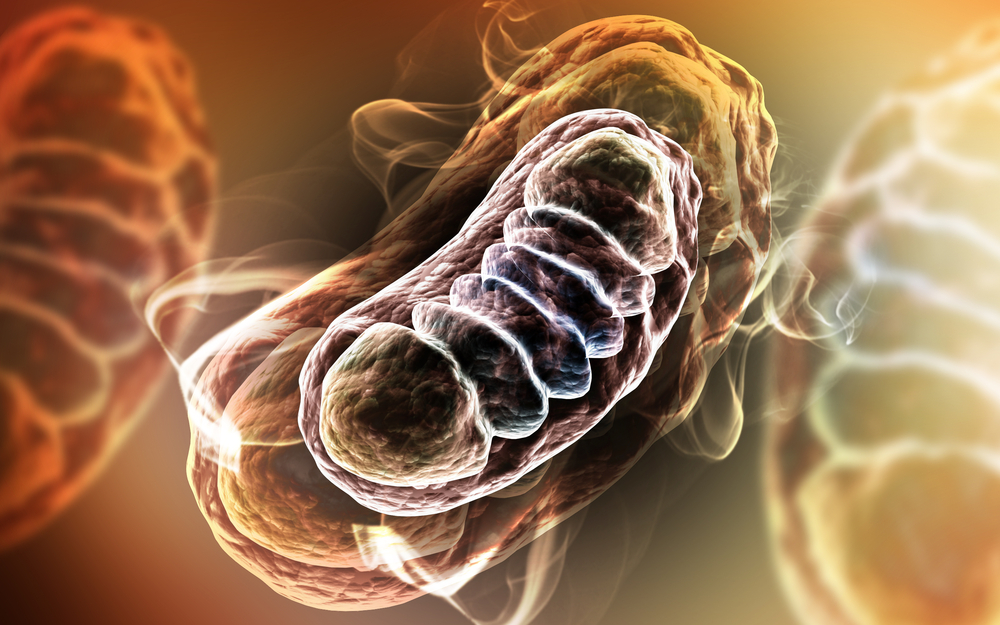
Specifically, they discovered that a kinase, AKT1, mediates mitochondrial ROS. Upon accumulation of these damaging molecules, cells activate an important protective mechanism known as mitophagy. Here, cells undergo selective degradation of mitochondria that are either dysfunctional or damaged.
“The biggest surprise was something that intuitively makes no sense: We show that mitophagy is required for TGF-β1 production,” the study’s senior author, A. Brent Carter, MD, a professor in the Division of Pulmonary, Allergy and Critical Care Medicine, UAB Department of Medicine, said in a press release.
When the team inhibited mitophagy in vitro, either by using a mitochondria-targeted antioxidant or by silencing Parkin2, one of the proteins necessary for mitophagy, they observed that TGF-β1 expression was abrogated. In agreement with these findings, mouse alveolar macrophages with a mutated Park2 gene also lacked TGF-β1 in bronchoalveolar lavage fluid. Importantly, mice carrying alveolar macrophages with a conditional Akt1 gene mutation or a conditional Park2 gene mutation underwent apoptosis (programmed cell death), and were protected against pulmonary fibrosis. These findings were also observed in human alveolar macrophages from IPF patients, with this cell type showing increased mitophagy and apoptosis resistance compared to normal controls.
In conclusion, the authors showed that Akt1-mediated mitophagy in alveolar macrophages induces apoptosis resistance and promotes TGF-β1 expression, two fundamental steps for pulmonary fibrosis development.







