Pulmonary Fibrosis Traced in Study to Failure of Lung Stem Cells to Regenerate
Written by |
Researchers may have discovered a key mechanism underlying pulmonary fibrosis (PF) — the failure of a particular group of lung stem cells to regenerate, hindering the repair of lung tissue in PF.
The study, “Hyaluronan and TLR4 promote surfactant-protein-C-positive alveolar progenitor cell renewal and prevent severe pulmonary fibrosis in mice,” was published in the journal Nature Medicine.
“Pulmonary fibrosis slowly robs patients of breath and finally life,” Paul W. Noble, MD, the study’s lead author, professor and chair of the Department of Medicine, and director of the Women’s Guild Lung Institute at Cedars-Sinai Medical Center, said in a press release . “In our study, we identified novel potential pathways to finding treatments for this relentless disease.”
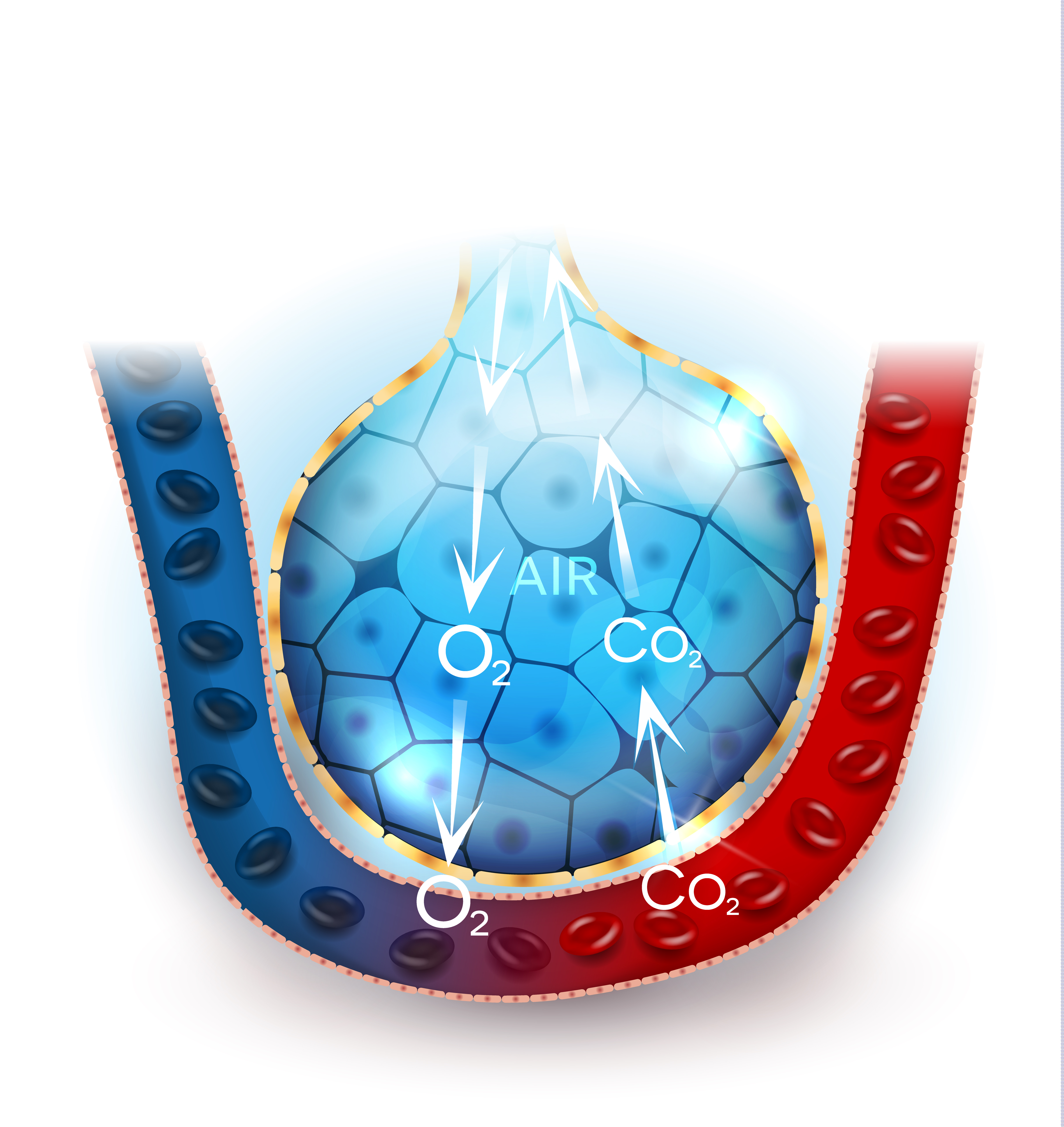
The team studied the alveoli, small air sacs in the lungs where the exchange between oxygen and carbon dioxide occurs. Airspaces must remain open for the lungs to work well, which is assured by a substance produce by epithelial cells lining the alveoli. In PF, these cells fail to function properly, leading to the buildup of fibrotic tissue and severe lung scarring.
Special stem cells in adult lungs, called AEC2s, are key to repairing and regenerating epithelial cells. In fact, whenever there is an insult to the lungs, through infections, pollutants, or other types of injury, AEC2s are vital in the repair process that follows.
Researchers discovered that AEC2s do not work as intended in PF. Looking at lung tissue from PF patients, they found fewer AEC2 cells overall, and those cells in evidence were less able to renew themselves compared to AEC2s in tissue from healthy individuals. Researchers also found that a natural chemical substance that promotes tissue repair and renewal, called hyaluronan, is present at much lower concentrations in AEC2 cells from PF patients.
The importance of hyaluronan was further demonstrated in mice, where its absence resulted in the type of scarring found in PF after lung injury.
“These findings are the first published evidence that idiopathic pulmonary fibrosis is primarily a disease of AEC2 stem cell failure,” said Carol Liang, MD, the study’s first author and an assistant professor of medicine at Cedars-Sinai. “In further studies, we will explore how the loss of hyaluronan promotes fibrosis and how it might be restored to cell surfaces. These endeavors could lead to new therapeutic approaches.”
Results suggest that targeting AEC2 cells in the lungs of PF patients and inducing their proliferation is a therapeutic strategy, Noble said.
“The exciting aspect is that we have learned how to isolate these stem cells from diseased lungs. We can use these cells to create tiny ‘lungs in a dish’ as tools for drug development,” Noble concluded.



