Targeting 2 Proteins in Lungs, Including Cannabinoid Receptor, is Potential Therapy for IPF
An investigative therapy for idiopathic pulmonary fibrosis (IPF) based on inhibiting two proteins, including the cannabinoid CB1 receptor, shows potential for halting fibrosis progression, and greatly improved survival in a mouse model for human IPF.
The study, “Cannabinoid CB1 receptor overactivity contributes to the pathogenesis of idiopathic pulmonary fibrosis,” was published in the Journal of Clinical Investigation.
The receptor, called endocannabinoid/cannabinoid receptor 1 (endocannabinoid/CB1R), previously was shown to reduce the promotion of fibrosis in multiple organs, including the liver, kidney, heart and skin. CB1R also has been linked to radiation-induced PF in mice and its activation is considered pro-inflammatory in chronic inflammatory diseases. The role of this receptor in IPF, however, remained largely unaddressed.
The fibrotic tissue in humans, as well as in mouse models of the disease, was shown to generate increased amounts of a molecule called inducible nitric oxide synthase (iNOS). It was found to strongly correlate with the degree of pulmonary fibrosis in human lung tissue, and inhibiting iNOS resulted in strong anti-fibrotic activity in animal models of PF. Overall, these data suggest iNOS is a potential therapeutic target for PF.
Now, researchers at the National Institutes of Health (NIH) investigated the impact of the endocannabinoid/CB1R system and its interaction with iNOS in human IPF and in the bleomycin-induced mouse model of PF, the most common experimental study model of human lung fibrosis. They investigated them as dual therapeutic targets.
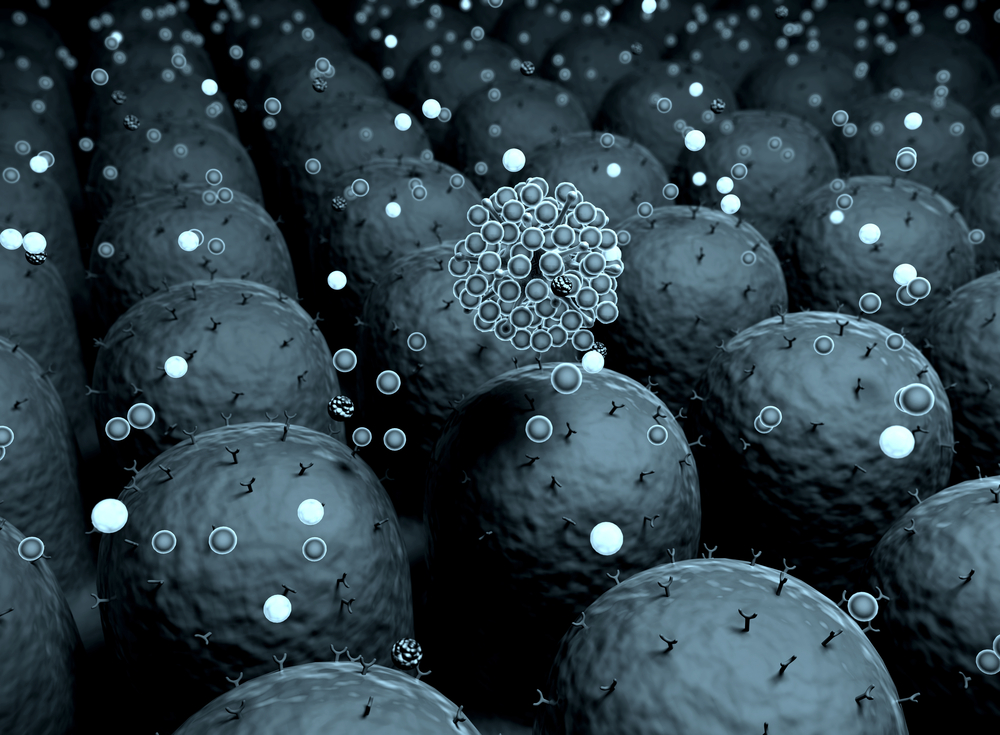
Researchers first analyzed lung fibrosis together with the endocannabinoid/CB1R system and iNOS in mice with bleomycin-induced PF. The same was performed using lung tissue and bronchoalveolar lavage fluid (BALF) from patients with IPF, along with healthy people, or controls.
They found a robust increased activity of CB1R, as well as one of its binding-molecules, called anandamide (arachidonoyl ethanolamide, or AEA) in lung and BALF samples from patients with IPF and from mice with BL-PF. These results suggest the endocannabinoid/CB1R system has an active role in IPF.
The role of the CB1R system was supported further with experiments using mice deleted for this system (called Cnr1–/–mice), which showed reduced bleomycin-induced fibrosis, improved survival, and decreased activation of alveolar macrophages. These are immune cells strategically positioned in the airways with an established role in PF.
The enzyme iNOS expression also was increased in both human IPF and in mice with BL-PF, and deleting the gene for this enzyme provided partial protection from BL-PF.
Overall, these results support both CB1R and iNOS in lung tissue as valuable therapeutic targets in PF. Researchers tested this approach, and inhibiting both proteins significantly reduced the progression of fibrosis and improved the survival rate of mice, when compared to inhibiting CB1R alone.
Most important, this dual inhibitory strategy completely arrested the progression of fibrosis in bleomycin-induced mice and improved their survival from 25% to 100%.







