4 Idiopathic Pulmonary Fibrosis Patients Share Their Stories
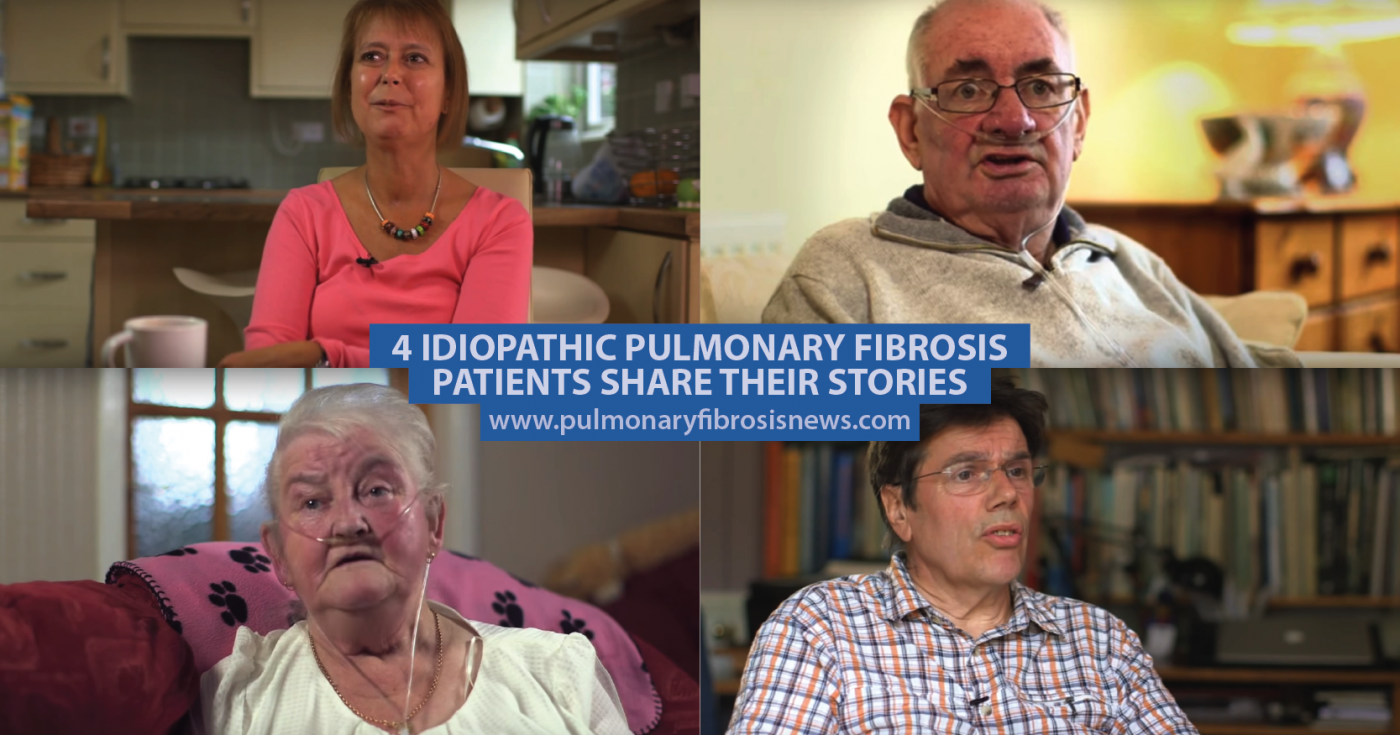
The British Lung Foundation has a series of videos featuring idiopathic pulmonary fibrosis (IPF) patients sharing their stories. The patients come from all walks of life and their journeys are all very different.
In this video, Joyce explains that it took four years before she received her idiopathic pulmonary fibrosis diagnosis. By the time she was diagnosed, the disease had progressed so much that she needed a double lung transplant. Joyce talks about her life before the lung transplant and how much it has changed for the better since the procedure.
MORE: Five questions about pulmonary fibrosis you should ask your doctor
Marilyn says her first symptoms of idiopathic pulmonary fibrosis were a constant cold and persistent cough. At first the doctor diagnosed depression, but hospital tests and X-rays showed that it was fibrosis. Following her diagnosis, Marilyn’s symptoms worsened quickly and she needed an around-the-clock supply of oxygen. However, oxygen therapy has improved her life and given her back some of her independence.
Seventy-five-year-old John first started developing symptoms of IPF in 2012 when he found it difficult to walk a short distance without getting breathless. His doctors first prescribed an inhaler but when it didn’t work, they sent John for a series of tests, including a lung X-ray which showed scarring on his lungs. Since being on oxygen therapy and other medications, John says he leads a fairly normal life, although he can no longer attend soccer matches.
Colin says the first sign that something was amiss with his health was breathlessness, which he’d experience when doing anything strenuous, along with pain in his chest. Doctors suspected angina, but tests revealed he had idiopathic pulmonary fibrosis. Colin manages his IPF with lifestyle changes and forward planning. So far he feels great but he takes it one day at a time.
MORE: Read about the five main factors for living with pulmonary fibrosis
Pulmonary Fibrosis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.






