Back Muscle Shrinkage Tied to Poor IPF Outcomes, Study Finds
A decline in back muscle mass is linked to poor clinical outcomes in patients with idiopathic pulmonary fibrosis (IPF), and can be used as an independent predictor of disease prognosis, a study found.
The study, “Early decrease in erector spinae muscle area and future risk of mortality in idiopathic pulmonary fibrosis,” was published in the journal Nature: Scientific Reports.
Difficulty breathing, decreased lung function, low blood oxygen levels during exercise, and lung tissue scarring visible in high resolution computed tomography (HRCT) scans are among factors that predict poor health outcomes in people with IPF.
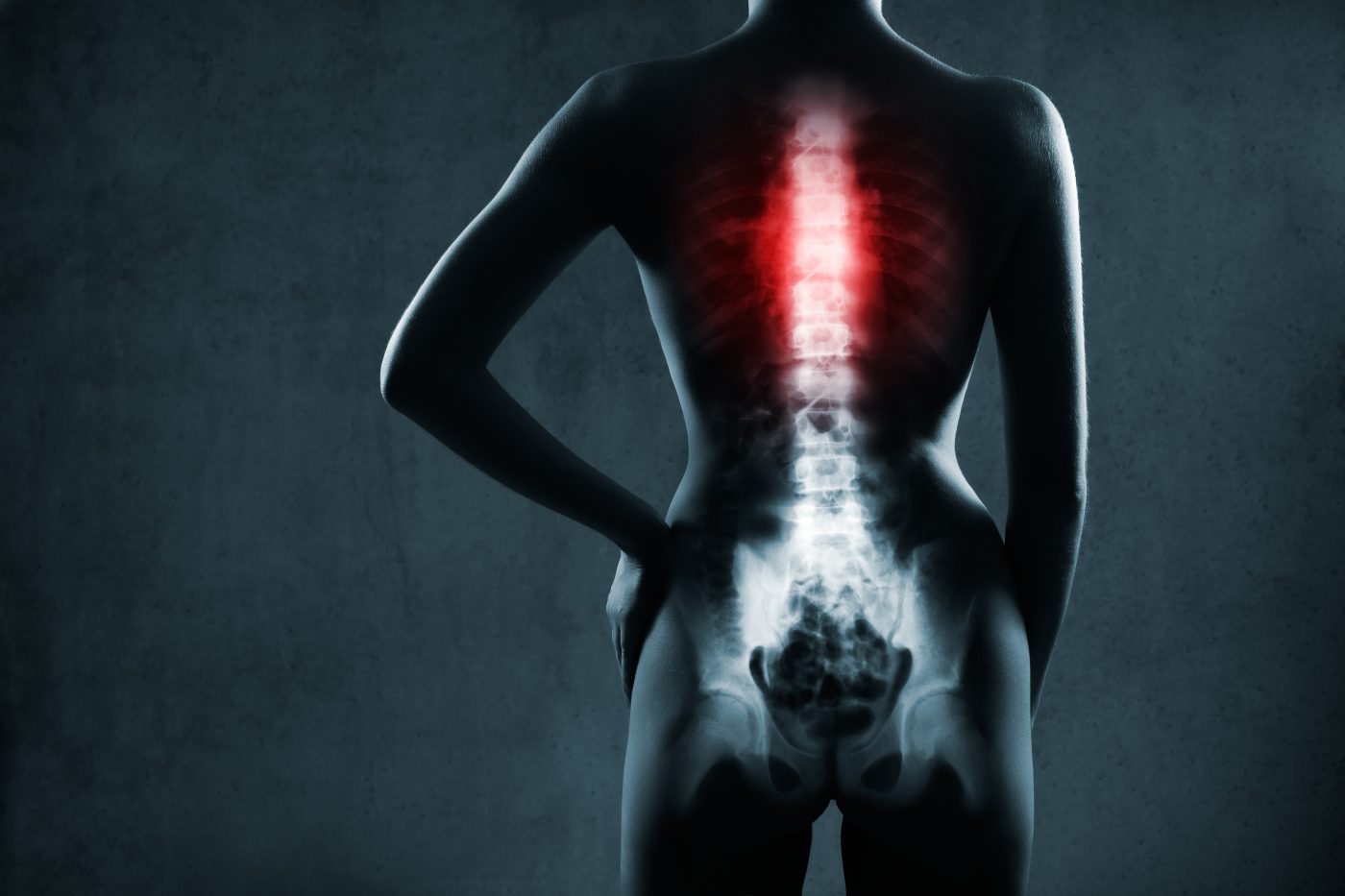
IPF patients also experience shrinking in the cross-sectional area of the erector spinae muscles (ESM), a group of muscles running along both sides of the spine. A study of patients with chronic obstructive pulmonary disease found the cross-sectional area (CSA) of these muscles to be an independent prognostic factor of the disease. A separate study reached similar conclusions for those with IPF.
Researchers at the Nagoya City University Graduate School of Medical Sciences and their colleagues looked at the medical records of 119 IPF patients who had undergone HRCT scans at referral and six months later. Scans were used to measure the CSA of the ESM around the 12th thoracic vertebra, just above the lower spine.
All patients had spirometry tests to evaluate lung function parameters, including forced vital capacity (FVC) and forced expiratory volume (FEV1). Gas exchange efficiency was assessed by the diffusing capacity of lung for carbon monoxide (DLCO). A six-minute walk test (6MWT) without oxygen supplementation was conducted to evaluate patients’ functional capacity.
Patient follow-up ranged from 817 to 1,633 days. Fifty-nine patients (49.6%) died during the study.
Findings revealed the decline in the ESM area was more pronounced than the FVC decline. This significant decrease in back muscles’ CSA was correlated with other clinical parameters, including FVC at baseline, lowest oxygen saturation (concentration) during the 6MWT, as well as with the relative decline in FVC, DLCO, and body mass index (BMI).
A statistical analysis found that, despite these correlations, the decline in the ESM area was the only significant prognostic factor that was associated with poor clinical outcomes.
An analysis to predict three-year mortality showed that those with ESM area declines of greater than 10.5% had a significantly poorer prognosis than those who had declines of less than 10.5%.
Patients with ESM area declines greater than 10.5% had lower BMI, FEV1, and oxygen saturation at baseline. They also had lower ESM areas after six months, shorter survival, and greater relative declines in ESM area, FVC, DLCO, and BMI.
No statistically significant differences in the relative decline of back muscle area was found between patients who were treated with corticosteroids during the study and those who were not.
“A reduced ESM CSA after six months was an independent prognostic predictor in patients with IPF,” the researchers wrote. “Early decrease in ESM CSA may be a useful predictor of prognosis in patients with IPF.”







