Explaining chronic illness to others? Try an elevator speech.
Time management, reading the room, and focusing on details are all helpful

Some of the most important interactions in our professional lives do not occur at work, at the boardroom table, or even in an office. Often, they occur during brief introductions or chance meetings.
The challenge for business leaders regardless of industry is how to briefly explain to someone what they do.
Years ago, I learned the art of developing an elevator speech. The concept is to create a concise description of what you do that can be shared during an elevator ride.
This challenge also applies to all of us with a rare disease. Sound easy? Let’s give it a try.
Details are important
I was diagnosed with idiopathic pulmonary fibrosis (IPF) in January 2017. When I was diagnosed, I knew little about the disease, so I quickly set out to learn as much as I could. My diagnosis was based on three indicators that are typical with IPF. The first was that my lungs had a distinctive crackle and appeared like ground glass on a CT scan. Next was a persistent and chronic cough. Finally, I had clubbed fingers.
The more I learned about IPF and what my future held, I began to refine what I shared. The story I was crafting had essential elements I would use over and over in a variety of settings, such as responding to questions from curious acquaintances, speaking at engagements as a Pulmonary Fibrosis Foundation Ambassador, and promoting awareness in the offices of federal lawmakers.
Engaging your audience
An immediate challenge of any exchange is engaging your audience. One of the first rules I recall learning about giving presentations is to read the room. To do this, think about the people you are engaging with and look for nonverbal cues, especially while you speak. Who is your audience? The message you deliver to a health aide for a member of Congress and the one you give to an audience unfamiliar with your disease are completely different.
Looking for nonverbal cues can be more challenging. People respond differently to information that is not a secret. If you are describing something particularly graphic, it may be triggering for someone and make them uncomfortable. At that point, they may stop listening.
Likewise, if a chance meeting allows you just two minutes, adjust your messaging to the available time. It is perfectly acceptable to offer additional information if a future meeting can be arranged.
Starting at a zero-knowledge baseline
If your diagnosis was familial pulmonary fibrosis, it’s likely that you had some knowledge of the disease before being diagnosed. In my experience, most people do not know about pulmonary fibrosis. Some will know the meaning of the two words but have little or no knowledge of the disease.
When I speak about IPF, I start with several basic terms to build my story: “chronic,” “progressive,” and “no cure.” These not only generate interest but also help to gauge it.
Leverage the outward indicators of your disease. Before I had a bilateral lung transplant two years ago, I went everywhere with oxygen. If people didn’t notice the E-sized tank of supplemental oxygen I had, they couldn’t miss my cannula. Since my transplant, I wear a hat to both protect me from the sun and because it displays pins showing that I am a Donate Life recipient. Any of these can be a conversation starter.
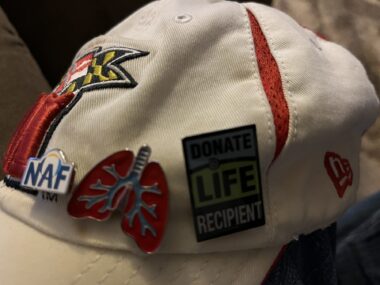
Hat pins are great conversation starters. (Photo by Sam Kirton)
The story
My audience for the following story might be a legislative health aide I meet somewhere off Capitol Hill:
“Are you familiar with idiopathic pulmonary fibrosis? It is a chronic, progressive lung disease for which there is no cure. There are two anti-fibrotic therapies that slow the progression, but they do not stop or reverse the disease. A lung transplant, if available, can improve the patient’s quality of life, but it comes with its own challenges. Despite the research being conducted today, more is necessary, and it is needed now. A future generation does not need to know about idiopathic pulmonary fibrosis. I need your member’s help to ensure it remains funded for the next fiscal year.”
Are you ready to create your own story? Feel free to develop, practice, and share it in the comments below. This way, we can all make every breath count.
Note: Pulmonary Fibrosis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Pulmonary Fibrosis News or its parent company, Bionews, and are intended to spark discussion about issues pertaining to pulmonary fibrosis.








Janice Moore
It seems so important to spread the word and information about this condition. People are unaware of its existence and shocked to learn of the predicted outcome. So any remarks of this type are most helpful.
Samuel Kirton
Hi Janice,
Thanks for reading my column and your comment. If each pulmonary fibrosis patient raises awareness with one person who then raises awareness with one person we could raise awareness in a relatively short period. I would love for you to come back and share your elevator speech.
Sam ...
Randall Thornton
Hello fellow IPF people. I know what you mean by people not knowing what IPF is,I didn't either when i was first told i had it. This was in March of 2020. I ended up staying in the hospital and rehab for 4 months. I had a surgeon take one look at me and said i know what's wrong with you and scheduled me for surgery. There she took out my right lung. After the surgery and she had a chance to diagnoiseit and then informed me about the disease. That is when i found out what IPF was and all the details about it. Now i tell people i have IPF and that is why i have to have oyxgen 24/7, they just look at you and don't get it. So, i get to explain to them about it. I get a wow or so sorry. I am asked how about a lung transplant. You have to be in better health then i am.
Samuel Kirton
Randy,
Thanks for reading my column and for your comment. I recognize you from the Forums. Can I ask where you are being cared for? Is there fibrosis in your left lung? How much oxygen are you on at this time?
Sorry for the questions but i think understanding your situation might help other readers.
Sam ...
Randall Thornton
Afternoon Sam, I am at home and doing as much as i can to help out my wife. I pretty much don't do anything outside anymore. I run out of air too soon to be much help out there. Again, i do what i can. I mostly help out inside then i am in the ac and don't have to worry about the heat and humidity. Dishes, laundry,clean the cat box and any other minor stuff that needs doing.
I am at 8 liters on the home compactor and 5 on the oxygen tanks when i go anyplace. I try to go someplace at least once or twice a week just to get out of the house. I am pretty much stuck at the altitude i am at now. I have tried going into the mountains and ended up passing out. My left lung is partially gone. On my last lung test, my results were 30% and that was hard to get. I guess at 20% you get put into hospice. I have another test coming up in Oct. so will see what that shows. Between my IPF and the heart troubles and coritus, i am on 22 pills per day. A second serving for breakfast and supper.
Well, that is it for now. Anymore questions, just let me know. Randy
Samuel Kirton
Randy,
Thanks for the response. Recognizing that you can only do what you can do is important. This disease changes the limits of what we can tolerate. Please come back on occasion or send me a note in the Forums to let me know how you are doing.
Sam ...
Maggi Liebig
Sam great jon on this article. Also, great how you answered everyones concerns. I look forward to see the new interview soon.
Maggi Liebig
Samuel Kirton
Maggi,
Thanks for reading my column and for your comments. I am glad you found value in the column. I learn so much from those who read the column and share their thoughts with me.
Sam ...