My IPF experiences have been like several genres of film
Even with horror and drama, I'm glad to now enjoy those Hallmark moments
Written by |

If your journey with pulmonary fibrosis were a movie, what best describes the genre? Horror? Comedy? Drama? Reality?
Wait, how about a Hallmark movie?
When I was diagnosed with idiopathic pulmonary fibrosis (IPF) in 2017, it was a complete surprise — and initially, best described as a horror movie.
My wife, Susan, was with me when Steven Nathan, a lung specialist, delivered the diagnosis. I processed it all quietly while Susan searched for it on the internet. The material she found was mostly negative. When I walked into the room, Susan would often begin crying.
We eventually found reputable sources of information, such as the Pulmonary Fibrosis Foundation and Pulmonary Fibrosis News, that led us to a better understanding of what we were facing and helped us transition out of the horror genre and move forward.
Meaningful movie moments
There have also been cinema-worthy moments when laughter was the best medicine.
When the team at Inova Fairfax Hospital here in Virginia was doing the work-up to determine if I qualified for a lung transplant, they needed to run a variety of labs. They once drew 29 tubes of blood in a single sitting. The total made quite an impression.
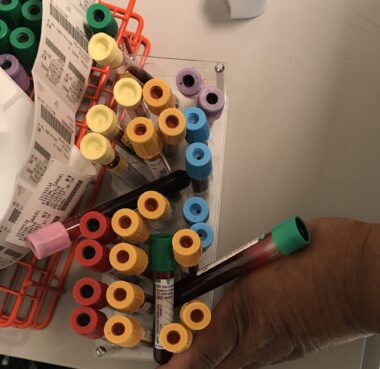
I do expect many readers to count the lab collection tubes. (Photo by Sam Kirton)
I also took a 24-hour pH manometry test, which records the levels of acidic and nonacidic reflux from the stomach into the esophagus. As part of this test, a thin, flexible probe is placed through the nose to travel to the stomach. It’s then connected to a device the patient has to carry for 24 hours.
My device was fit and then removed at Inova Children’s Hospital, where the waiting-room furniture was, naturally, pediatric-size. Walking back to the clinic on the day I completed the test, I encountered a young child and his mother. He smiled, seeing that we were having the same test.
At times on my journey, I also had sobering encounters with reality — and not a shortage of them, either. Here are a few examples of that genre to help clarify what it’s like.
During COVID-19 in 2020, for instance, Susan and I met with a local funeral home to make my funeral arrangements and pay for them. I signed the check myself.
As my IPF accelerated, my care team let me know that I was in the window for a lung transplant — and without one, I likely wouldn’t see Christmas 2021.
I got the call at 9:03 a.m. on July 9, 2021, explaining that my care team had lungs for me and I needed to come to the hospital. In the immediate moments after I hung up the phone, I realized that someone had just passed away and I was going to receive their gift of life. That caused me to pause. Susan and I said a prayer for my donor and donor family before we even moved from the spot where we’d received the call.
Following my bilateral lung transplant on July 10, 2021, my next brush with reality came when I was being extubated, or when the tube was removed from my airway. Susan was talking to me as I emerged from the fog of anesthesia about 29 hours after the transplant. She asked me if I was ready to breathe, and I was shaking my head no. In my mind, if this procedure didn’t work, there was no going back. Once I took those first few breaths (which Susan recorded on video), I knew all would be OK.
The movie moments continue to occur almost daily, and some have touches of that Hallmark genre.
I’ve gotten to see Abigail, my oldest granddaughter, grow up and start school. Her sister Charlotte was born about a month after my transplant. Their youngest sister, Brooklyn, is now 1 year old.
Today I feel that every conversation I have with a newly diagnosed patient is one of the reasons I was blessed with a transplant.
I even feel blessed seeing a sunrise with my coffee, or a sunset while walking my dog, Beau.
The lens through which you view your journey is important, especially with pulmonary fibrosis. There will be times when all sorts of emotions will be present. Some may appear briefly while others may linger longer than you’d like. Call on others during dark times and celebrate all the movie moments. I know it’s helped me make every breath count.
Note: Pulmonary Fibrosis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Pulmonary Fibrosis News or its parent company, Bionews, and are intended to spark discussion about issues pertaining to pulmonary fibrosis.








Gam
Hi Samuel, quite a story. I was diagnosed with IPF at the end of 2018 when I had double pneumonia. I took lung function tests every 6 months but nothing was prescribed. My doctor held back on prescribing OFEV as the side effects sounded really bad. But in April 2024 just back after a visit to India I had to be rushed to emerg for sob. Since July 2024, I have been going through some very troublesome days, sometimes doubting I would get through the day. My doctor still thinks I'm not eligible for a lung transplant. I guess criteria for lung transplant is different here in Canada. Each day gets harder and harder but I try to keep busy with household stuff.
I do have my next appointment with my respirologist at the end of July 2025 and hopefully I can ask him again for a lung transplant recommendation.
Samuel Kirton
Hi Gam,
Thanks for reading my column and your comment. I hope you will come back and let me know how you are doing.
Sam...