Meeting the 3 Requirements for Hospital Discharge After Lung Transplant
Written by |

On Aug. 14, 2020, around 10 p.m., my successful lung transplant was completed. Now I was in the daunting recovery phase. Before being discharged from the hospital, I had to meet three requirements:
- Walk 1,000 feet without supplemental oxygen.
- Walk continuously on a treadmill for 30 minutes.
- Have all my chest tubes removed.
After hallucinating and fainting on my first day of recovery, I wondered what would go wrong while accomplishing these tasks.
Walk 1,000 feet
On Aug. 16, the physical therapist (PT) took me for a walk in the hallway.
Imagine having four chest tubes connected to a chest tube drainage system, an IV pole, and an oxygen tank, then trying to go for a walk. It challenged me because of all the equipment. I pushed a wheelchair that held the chest tube drainage systems and the oxygen tank. The PT had the IV pole, and another nurse pushed a chair behind me.
I went 100 feet. It wasn’t far, but I wasn’t too concerned because it was my first walk with new lungs. Because I had my transplant during the pandemic, I had to be extra careful to protect my immunocompromised body. Wearing a mask made it difficult to breathe and to walk.
The next day I walked farther, but it was only 220 feet. At the end of my walk, I was tired and a little lightheaded. Later, I found out I had gone into atrial fibrillation.
These results were discouraging. My goal was to be discharged within two weeks, but I believed I wouldn’t be able to accomplish it.
On Aug. 18, my walk was different from the previous days. Instead of pushing a wheelchair, I used a walker with wheels that didn’t work. I walked 320 feet. It didn’t feel like an accomplishment to walk farther, even with more restrictive tools.

An improvised mask insertion can help make breathing easier following transplant. (Photo by Kevin Olson)
Finally, on Aug. 19, I walked 1,000 feet without stopping. The physical therapist gave me a great tip that made it easier to breathe while walking: She said to use a small cup with the end cut off inside the mask. This cut down on the hot air and made a world of difference.
I met the first requirement. Then, the doctors ordered the discharge education training to begin. I had high hopes of being discharged on Friday, Aug. 28. I was ready to take on the treadmill.
Walk on the treadmill for 30 minutes
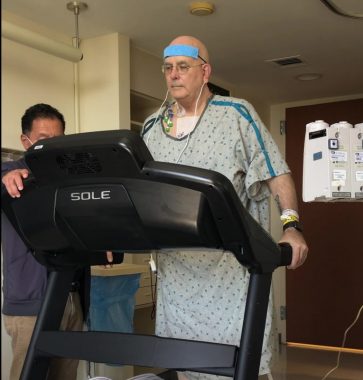
Kevin Olson walks on the treadmill as part of post-transplant recovery in August 2020. (Photo by Dana Olson)
The following day, I attempted the treadmill walk. When I stood up to get on it, my chest tube dressings started to fall off. They were soaked because my incision had two small holes draining fluid. However, the leaks didn’t hamper my pulmonary rehabilitation. As I walked, more bandages kept falling off, and liquid fell onto the treadmill belt. My wife said the pulmonary rehabilitation technician kept wiping off the belt.
Although it was messy, I completed my 30-minute walk on the treadmill on my first try. My discharge education appointments were scheduled for Monday and Tuesday, three days before I hoped to be discharged. I was delighted about the possibility of discharge on Aug. 28.
Chest tubes removed

The Shadow Buddies Foundation provided Kevin Olson with a lung transplant Buddy to help explain the various procedures. (Photo by Kevin Olson)
I had four chest tubes. You can see their approximate position below the clamshell incision on my lung transplant Shadow Buddy, pictured above.
The nurse practitioner pulled the two interior tubes on Aug. 16. I was ecstatic because I believed the others would be out soon.
The two small holes in my incision hampered getting the last two tubes removed. My surgeon said they would heal up with no problems. However, every time I sat down in the chair, my chest sounded like a whoopee cushion.
On Aug. 31, a nurse practitioner pulled my right chest tube. Unfortunately, they had to put in a right-side pigtail chest tube a couple days later. The reinsertion of a chest tube was demoralizing, which increased my depression. It frustrated me to take one step forward and two steps backward.
On Sept. 3, I had an exploratory wound surgery that fixed my incision issue. Initially, I worried about having another surgery, which to me represented another setback.
On Sept. 11, the final chest tubes were taken out, ticking the last box required for me to go home.
Discharged!
Thirty-one days after my transplant surgery, I was finally able to say, “The eagle has landed!” I was discharged from the hospital and went to our apartment on Sept. 14. To celebrate, I drank my first post-surgery “wine,” which was actually just a bottle of water. Nevertheless, I felt human again.

Kevin Olson toasts with a bottle of “wine,” which was really water, after being discharged from the hospital on Sept. 14, 2020. (Photo by Dana Olson)
Time in the hospital can significantly vary for everyone. My stay was longer than I’d hoped, but I know two people who only stayed in the hospital for a week. Others stayed longer than me.
What was your experience preparing for hospital discharge like? Please share in the comments below.
***
Note: Pulmonary Fibrosis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Pulmonary Fibrosis News or its parent company, Bionews, and are intended to spark discussion about issues pertaining to pulmonary fibrosis.





majid
Hi, sir I, m very happy God give you new life, God bless you always, my father also right lung fibrosis patient and my father age is now 83 year old, what can I do my father back in normal life please guide me sir
Kevin Olson
Thank You for reading my column. Prayers for your father and you.
Michael Moses
I an 72 and had a single lung transplant on March 16th, 2021. My stay in the hospital was 18 days. This was the first time I was ever admitted to a hospital (lots out outpatient over the years). I decided beforehand that my stay would be somewhere between 2 weeks and 6 months. I was doing extremely well (so everyone told me) and was ready to come home on the 14th day, but my potassium and magnesium numbers were off which took another three days to get under control. Exercise is very important, both before and after surgery. Also being overly careful of germs, etc. I was fine until about a month ago when I developed a cold and diarrhea. Then my kidney was acting up. It has taken over a week to get this under control with changes in meds and hydration twice. It is an ongoing process. Hopfully, my meds will find a "good place" in the coming months. Overall, I believe that I am still very fortunate and lucky. The best is yet to come. My advice is to keep a good outlook, follow directions on meds and tests and exercise.
Kevin Olson
Michael. Sorry for the late response. Thank you for sharing your journey. I was 66 when I had my transplant. My surgeon said it would take a year to recover fully. I am at my one-year mark and doing great. I understand about your body adjusting to the meds. After a year, I am at the point where my meds don't change weekly or bi-weekly. Also, I don't have labs drawn weekly. I do my labs every two months now. Keep up the great work. Thank you for reading my column.
Ronald Cole
Kevin thank you for sharing your 30 day journey. It does give me hope as I am going through pre transplant. Getting the "Million" door work up. I'm 62 years old and good health except for IPF. Trying to keep a positive attitude and a can do spirit. I hope you can share more of you progress and a out taking anti rejection drugs.
Ron
Kevin Olson
You are welcome, Ronald. It is great to hear that you are in good health other than the IPF. So that, your age 62 and positive attitude will be a plus for a transplant. For me, in my transplant evaluation, I experienced many unexpected road bumps, which were frustrating. Your attitude will help with those road bumps. Just Expect the Unexpected and quickly get over the unexpected. Last, I will be writing more columns over time about my transplant experiences. Thank you for following me.