What happened after COVID-19 finally caught up to me
A transplant recipient explains what COVID-19 treatment looked like for him
Written by |

American comedian Bill Engvall is known for his punchline “Here’s your sign,” which he’d often say in response to an outrageously obvious question. I recently experienced two “here’s your sign” moments of my own after wondering if I’d contracted the virus that causes COVID-19.
On Monday, April 3, I started experiencing extreme chills, a headache, and body aches during a flight from Las Vegas to Washington, D.C. I took a COVID-19 antigen test in the parking garage at a Washington airport, and it indicated “positive” before I could even set it down. That was my first sign.
COVID-19 — really?
For more than three years, my wife, Susan, and I had avoided COVID-19. That record is now spoiled.
Given my history with idiopathic pulmonary fibrosis and a bilateral lung transplant, I immediately paged the on-call lung transplant coordinator at the Inova Fairfax Hospital’s Advanced Lung Disease and Transplant Center in Virginia. I heard back from her in less than 10 minutes.
After taking note of all the symptoms I was experiencing, she passed the information along to the on-call pulmonologist at the clinic. Within minutes, I received another call telling me to go to Inova’s emergency department and plan on being admitted.
Admission
Doctors there confirmed the positive COVID-19 test, treated the nausea caused by my coughing, and drew multiple labs to identify any additional issues we needed to address.
I was isolated in a room on the fourth-floor cardiac telemetry unit, which is where I spent many days after my transplant in 2021, as well as during my bout with pneumonia in late September 2022.
That was also where I received my second sign: A notice was posted in my room indicating I was under airborne and contact isolation with eye protection. The back of the sign noted that these precautions should be taken when a patient has an infectious disease like SARS-CoV-2 or Ebola.
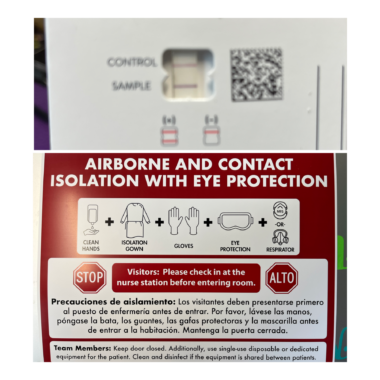
“Here’s your signs” that I had COVID-19. (Photos by Sam Kirton)
Post-transplant COVID-19 treatment
As a solid organ transplant recipient, I take a variety of drugs every day that suppress my immune system to prevent rejection of my donor’s lungs. For that reason, doctors decided to give me three infusions of Veklury (remdesivir), a medication used to treat COVID-19 patients, while I was in the hospital.
I was admitted on Monday night, and my infusions took place on Tuesday, Wednesday, and Thursday. I began to feel better after the first infusion.
I hadn’t eaten a meal since Sunday evening, as I had no appetite on Monday morning and became nauseous later that day. I felt better on Tuesday, but I paced myself so as not to upset my stomach. I was able to get out of bed on Wednesday and spent my time sitting in a chair. My exercise was limited to my hospital room.
I feel it’s also important to mention that I used supplemental oxygen for days, as my oxygen saturation percentages dropped to the mid-80s due to COVID-19. I was taken off supplemental oxygen on Wednesday, and my care team conducted a walk test to ensure I didn’t drop to unsafe levels during exertion.
Going home
I was discharged on Friday afternoon and was allowed to drive myself home. My discharge instructions included a high dose of prednisone, which tapered to an end after a week, and isolation at home.
The isolation period lasted through the following Friday, April 14. After that, I was clear to resume my normal activities. I also learned I shouldn’t expect a negative COVID-19 test because of my suppressed immune system.
A happy ending
There’s some irony to this story. On April 10, the U.S. ended the national emergency related to the COVID-19 pandemic. However, this action shouldn’t be considered an all-clear. As my experience demonstrates, the world isn’t done with COVID-19.
Those in the pulmonary fibrosis community should continue to take precautions to protect their health. Do what’s necessary to feel comfortable and safe in your environment. Your health must be your priority.
I won’t let COVID-19 turn me into a recluse. I’ll talk with my care team about precautions I can take to help me stay healthy. My donor’s lungs gave me the gift of life, and living it is how I make every breath count.
Note: Pulmonary Fibrosis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Pulmonary Fibrosis News or its parent company, Bionews, and are intended to spark discussion about issues pertaining to pulmonary fibrosis.







Steve Dragoo
I know Innova well having lived in FX 35 years. Currently going through my second acute exacerbation and at first thought it was covid but the symptoms changed so - no test desired/needed. Couldn't work for 3 weeks and hope to avoid covid when we return stateside soon - buutttt...
Stay well...
Steve
Samuel Kirton
Steve,
Thanks for reading my column. I recognize your name as a regular reader here at Pulmonary Fibrosis News. I am now 19 months post-transplant and this is my 2 nd exacerbation. The 1st was pneumonia during September 22 and COVID this month. Any type of respiratory event is not something to be taken likey for me. I will continue to be mindful and mask up when it is the best choice for me.
Sam ...