C21 Improves Lung Function in IPF Patients During Phase 2 AIR Trial
Written by |
C21 (VP01), Vicore Pharma’s investigational oral therapy, safely and effectively improves or stabilizes lung function in previously untreated adults with idiopathic pulmonary fibrosis (IPF), according to interim data from the open-label Phase 2 AIR trial.
“Based on the mechanism of action of C21, which has both vascular and [anti-scarring] characteristics, we were optimistic, but this exceeds our expectations,” Joanna Porter, MD, PhD, the trial’s coordinating investigator and a professor of respiratory medicine at University College London, said in a press release.
“This is very encouraging data,” said Toby Maher, MD, PhD, a clinical expert at Vicore and a professor at Imperial College London and the University of Southern California’s Keck Medicine.
“To see stabilization in patients over 36 weeks is certainly not something we would expect to see by chance in a clinical trial and definitely warrants further assessment of C21 in IPF,” Maher added.
Based on these positive early findings, which were further detailed in a company webcast, Vicore is planning to launch a Phase 2b dose-finding trial, called AIR 2, to confirm these results and accelerate C21’s development in parallel with the AIR study. AIR’s top-line data are expected in the last months of this year.
“Now that the interim analysis has shown both safety and a positive effect on lung function in this trial, we want to move as quickly as possible to the next stage to be able to bring this treatment to patients,” said Rohit Batta, MD, Vicore’s chief medical officer.
C21 is a first-in-class, small-molecule activator of angiotensin II receptor type 2 (AT2R), a protein receptor whose activation promotes blood vessel widening and prevents tissue scarring, or fibrosis, by activating the “protective arm” of the renin-angiotensin system.
AT2R is found at the surface of alveolar type 2 (AT2) cells, one of the cell types that line the small air sacs responsible for gas exchange in the lungs and that are involved in lung tissue repair and regeneration. Dysfunctional AT2 cells contribute to lung fibrosis.
By activating AT2R, C21 is designed to improve blood flow and reduce the formation of scar tissue in the lungs, ultimately slowing or preventing further IPF progression.
Previous data showed the therapy effectively reduced lung fibrosis in animal models and blocked the activity of TGF beta-1, a major pro-fibrotic molecule, in lung tissue samples from an IPF patient.
C21 received orphan drug designation in the U.S. and Europe for IPF. The designation is meant to accelerate the therapy’s development and review by providing financial benefits and regulatory support. It also provides a marketing exclusivity period, of seven years in the U.S. and 10 years in Europe, upon approval.
The proof-of-concept AIR study (NCT04533022), which enrolled its first patient in November 2020, is evaluating the safety, pharmacokinetics, and effectiveness of C21 in about 60 adults, 40 or older, with IPF who had not received prior disease-specific treatment. Pharmacokinetics refers to the therapy’s movement into, through, and out of the body.
Participants, recruited at sites in the U.K., India, Ukraine, and Russia, receive a 100 mg oral capsule of C21 twice daily for 24 weeks (nearly six months). They may choose to continue treatment for an additional 12 weeks, totaling nearly nine months of treatment.
AIR’s main goal is to assess the frequency and severity of adverse events, as well as changes in forced vital capacity (FVC), a standard lung function measure, over the course of the study.
At the time of the interim analysis, 21 participants had evaluable data: 13 had been treated for three months, nine for nearly six months, and seven for nearly nine months.
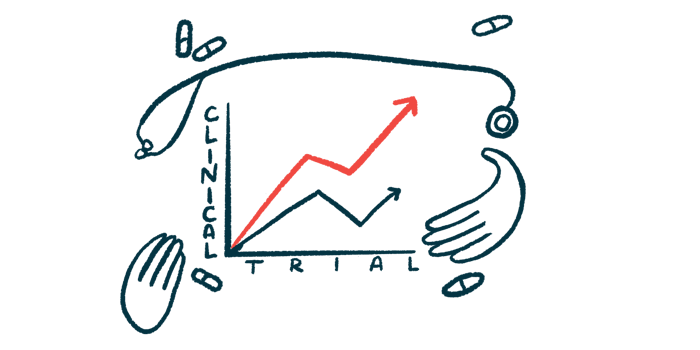
Results showed that FVC remained generally stable up to about 18 weeks of treatment (just over four months), after which it was markedly increased, indicative of better lung function.
Patients treated for nearly six months had a mean increase of 251 mL in FVC, which contrasted with the expected FVC decline of 120 mL in untreated patients over the same period of time — a significant difference of 371 mL.
Also, between six and nine months of treatment, FVC continued to improve in five of the seven patients, and remained stable in the other two. C21-treated patients showed significantly different FVC slopes at 28 weeks (over six months), 32 weeks (about 7.5 months), and 36 weeks (nearly nine months) compared with what would be expected for untreated patients.
The therapy was generally safe and well-tolerated, causing no treatment-related serious adverse events, sudden periods of disease worsening, or gastrointestinal problems.
These interim findings suggest that C21 is generally safe and that it improves lung function in previously untreated IPF patients.
Vicore is also testing C21 as a potential treatment for COVID-19 and systemic sclerosis, an autoimmune disease characterized by tissue fibrosis.
In addition, the company is working on the development of two other IPF candidates: VP02 (inhaled thalidomide) for IPF-related cough, and VP04, a digital cognitive behavioral therapy for depression and anxiety associated with IPF. According to the webcast, clinical trials for both of these candidates are expected to start this year.