Engineered stem cells could regenerate damaged tissue in PF
Stem cells are precursors from which other specialized types of cells are derived
Scientists have developed a way to use engineered specialized stem cells to regenerate healthy airway tissues, offering a potential avenue for treating chronic lung diseases like pulmonary fibrosis (PF).
In a pair of proof-of-concept preclinical studies published in Cell Stem Cell, scientists described how they engineered lung stem cells and then used them to repopulate lungs with healthy cells in mouse models of lung injury.
Making specialized lung stem cells in the lab may rely on induced pluripotent stem cells (iPSCs), which are reprogrammed stem cells first obtained from adult cells that can be turned into virtually any other cell type under the right conditions.
“We hope this work will help to pave the way toward developing new therapeutic approaches where iPSCs can be made from any patient with lung disease, differentiated into lung stem cells in the laboratory, and used for transplantation to reconstitute the healthy airway … in a way that is durable and functional,” Martin Ma, a doctoral student at Boston University and the first author of one of the papers, said in a university press release.
Starting with stem cells to treat pulmonary fibrosis
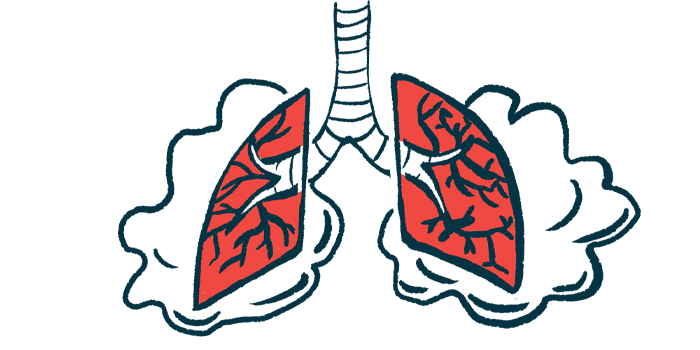
Stem cells are the body’s source materials and serve as precursors from which other specialized cell types are derived. They help keep tissues healthy by replenishing cells lost during normal cellular turnover and after injury. Scientists believe they could be leveraged for lung diseases like PF, where chronic inflammation and scarring cause progressive lung damage and respiratory function declines. The goal would be to populate stem cell compartments in the airways, allowing them to continuously regenerate important lung cells that’ve been lost or damaged.
Researchers from the Center for Regenerative Medicine (CReM), a joint venture between Boston University and Boston Medical Center, have been working on a way to do this over the last two decades.
In the first study, “Airway Stem Cell Reconstitution by Transplantation of Primary or Pluripotent Stem Cell-Derived Basal Cells,” the researchers described the process of developing and transplanting stem cells engineered to regenerate cells of the airway epithelium, those that line the airways.
Using different types of human or mouse stem cells, scientists could prompt these general stem cells to transform into airway basal cells — specialized stem cells of the airway epithelium.
When transplanted into the airways of a mouse model of airway epithelial lung injury, these basal cells demonstrated lifelong engraftment. In other words, they remained in the airways and were able to continuously renew themselves, giving rise to functional airway epithelium cells for years.
“Because the cells engrafted as basal cells, the normal stem cell of the airways, they were able to self-renew or make copies of themselves by dividing and also giving rise to other cell types that together make a functional airway epithelium,” said Darrell Kotton, MD, professor at Boston University, CReM’s director, and the study’s corresponding author.
In the second study, “Durable alveolar engraftment of PSC-derived lung epithelial cells into immunocompetent mice,” the researchers sought to regenerate cells of the alveoli, or the tiny air sacs in the lungs where gas exchange occurs.
The engrafted stem cells were able to produce both alveolar type 1 and type 2 cells. While type 1 cells are the major cells involved in gas exchange, type 2 cells are their precursors. By giving rise to both types, the strategy ensures that cells in the alveoli retain their function and ability to self-renew in the long term.
“Collectively, these two publications mark a significant methodological step forward toward making iPSC-based lung regeneration a viable treatment approach for a variety of lung diseases in the future,” said Jim Kiley, PhD, director of the Division of Lung Diseases at the National Heart, Lung, and Blood Institute, which funded the work.
Why using iPSCs is easier
While directly taking specialized stem cells from the airways of a donor could repopulate lung tissue, using iPSCs is easier since the necessary cells can be obtained from a blood or skin sample and then reprogrammed in the lab to produce larger quantities of the target cells.
In genetic conditions, a person’s own stem cells could be engineered to correct the genetic defect before being given back to patients, granting yet another advantage to this therapeutic approach and bypassing the need for immunosuppressant treatment, which is required with a transplant.
“Since these cells will be the patient’s own cells … in theory they should not be rejected after transplantation … thus avoiding any need for immunosuppression, as we have demonstrated in our two proof-of-concept … studies,” said Michael Herriges, PhD, a postdoctoral researcher at Boston University and first author of the second paper.
The road to clinical development for nongenetic diseases like PF may still be a long one.
“Treatment of lung diseases like emphysema, pulmonary fibrosis and COVID-19 will take a lot more research,” Kotton said.