Green and glowing mouse lung cells made to model PF in the lab
The cells will let researchers study how lung diseases develop
Written by |
Researchers in the U.S. turned a special type of mouse stem cell into green, glowing lung cells in the lab and now have a limitless supply they can use as a model to study how pulmonary fibrosis and other lung diseases develop.
“Our study has implications for the study of lung diseases, such as pulmonary fibrosis and interstitial lung diseases that arise from dysfunction of the part of the lung known as mesenchyme,” Darrell Kotton, MD, who led the study, said in a university news release. Kotton directs the Center for Regenerative Medicine of Boston University and Boston Medical Center and is a David C. Seldin professor of Medicine at Boston University. “These diseases currently have very limited treatment options and we hope our model system will provide new tools to understand what goes wrong in these diseases and to screen for better drugs,” Kotton said.
The study, “Directed differentiation of mouse pluripotent stem cells into functional lung-specific mesenchyme,” was published in Nature Communications.
Pulmonary fibrosis occurs when lung tissue becomes scarred and thickened, making it difficult for oxygen to pass through the lungs into the bloodstream.
What causes lung tissue to undergo these changes is unclear and it can be difficult to collect cells directly from the lungs. To get around this, researchers generated a special line of mouse-induced pluripotent stem cells (iPSCs).
Turning iPSCs into lung cells, green and glowing
Stem cells can give rise to many different cell types. These had a mesenchymal-specific tag added to their genetic code. This tag, which glows green under fluorescent light, lets researchers trace the iPSCs that were turning into lung mesenchymal cells as they developed. Lung mesenchymal cells are a component of lung tissue that play key roles in normal lung development and disease. They’re also involved in tissue repair and recovery following an injury.
The researchers didn’t know what made iPSCs turn into lung cells, so they tested different substances. They found the combination of retinoic acid and purmorphamine yielded the highest percentage of green fluorescent cells. Retinoic acid is made naturally from vitamin A. It may help repair damaged lung tissue in mice with idiopathic pulmonary fibrosis. Purmorphamine activates the Hedgehog pathway, a signaling cascade that’s important for embryos to develop, but is overactive in pulmonary fibrosis.
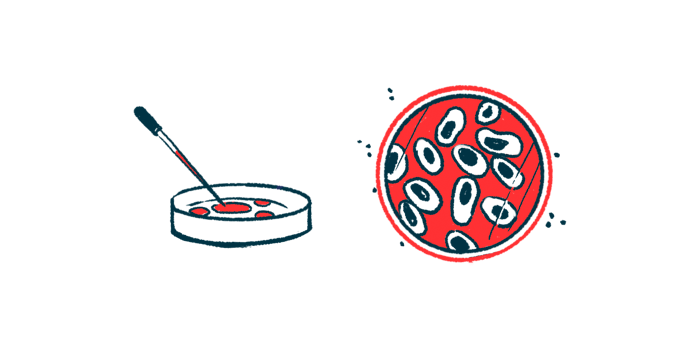
To see if the green glowing cells resembled those from the lung mesenchyme of mouse embryos, researchers looked at which genes were turned on and which were off, focusing on markers of lung mesenchyme.
The levels of most of the markers peaked around 10-12 days after the iPSCs began morphing into other cell types. Moreover, the levels of 12 of 15 of these lung mesenchymal markers were similar to those of lung cells harvested from 12.5-day-old mouse embryos.
While the glowing green cells looked like lung cells, researchers wanted to test if they functioned as lung mesenchyme. To do this, they assessed their ability to form organized 3D structures called organoids.
These organoids had layers of lung mesenchymal cells and lung epithelial cells, similar to how lung tissue is structured in the body. Epithelial cells are a type of cell that cover the body’s surfaces. Grown together, they influenced each other’s development, suggesting communication between the two types.
“An important role of the developing lung mesenchyme in the experimental model is their ability to interact with and signal to the neighboring epithelium,” said Andrea Alber, PhD, a postdoctoral fellow in Kotton’s lab and the study’s first author. “We found that our engineered cells can recapitulate some of those signaling interactions, suggesting that they have functional capacity. We are now working to apply these types of new organoid models to better understand pulmonary fibrosis.”
“To study human lung mesenchyme development and to model human respiratory diseases involving the mesenchymal lineage, such as pulmonary fibrosis, establishing a protocol for the differentiation of human iPSCs into lung mesenchyme will be crucial,” the researchers wrote.