Metformin, for Diabetics, Effectively Treats Models of Silica-induced PF
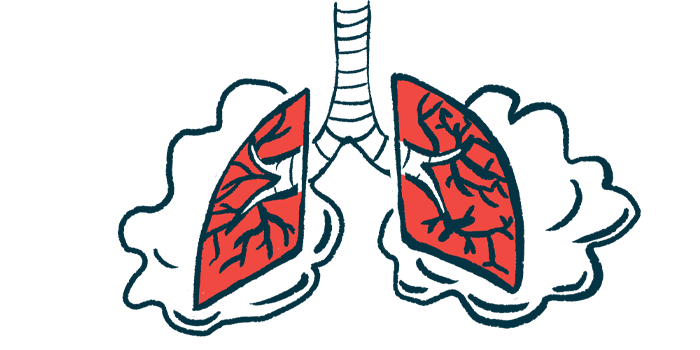
A type 2 diabetes medication, metformin significantly eased lung inflammation and scarring (fibrosis) in a mouse model of silica-induced pulmonary fibrosis (PF), both at early and late stages of the disease.
Notably, these benefits were found to be associated with a reduction in oxidative stress, inflammation, fibrotic markers, and maturation of lung fibroblast cells into myofibroblasts — the main drivers of PF. (Oxidative stress is an imbalance in the production of reactive oxygen species, harmful molecules that can damage and kill cells, and are associated with fibrosis.)
These findings support metformin, likely in an inhaled formulation, as a potential therapy for silica-induced PF, the researchers noted.
The study, “Metformin attenuates silica-induced pulmonary fibrosis via AMPK signaling,” was published in the Journal of Translational Medicine.
Silicosis, one of the most common occupational causes of PF, results from repeatedly inhaling fine particles of silica, a common mineral found in sand, quartz, and many other types of rock. The condition is typically associated with construction, sandblasting, and mining.
“Although efforts to improve the work environment have been made for years, the incidence and prevalence of silicosis worldwide have been rising, especially in developing countries like China,” the researchers wrote.
However, the underlying mechanisms of silicosis remain poorly understood, and few treatments to date can effectively “halt disease progression or reverse established lung fibrosis,” highlighting the “urgent need” for efficient therapies, the researchers added.
Metformin, a common oral treatment for type 2 diabetes, was previously shown to have protective effects in several lung diseases by suppressing inflammation, lessening oxidative stress, and affecting fibroblast-to-myofibroblast transition.
Notably, a 2018 study reported that metformin could reverse established lung fibrosis in a mouse model of PF and in lung tissue from IPF patients in an AMPK-dependent way. AMPK is an enzyme that works as a key regulator of energy metabolism and balance.
Now, a team of researchers in China evaluated the anti-fibrotic effects of metformin in an induced mouse model of silicosis, and in lab-grown cells exposed to silica-based particles or TGF-beta 1, a known driver of PF.
These cells included lung epithelial cells (those that line the lungs), macrophages (a type of inflammatory immune cell involved in lung fibrosis), and lung fibroblasts.
Researchers treated the mice for two weeks with metformin at 100 or 300 mg/kg, starting either one day after silica exposure (early stage of fibrosis) or 28 days later (late stage of fibrosis).
At the high dose, metformin was seen to significantly reduce the severity of lung lesions and the degree of their distribution, as well as the levels of several fibrotic and inflammation markers at both early and late disease stages.
Notably, these reductions often resulted in levels closer or even lower than those found in healthy mice.
Further analyses in lab-grown cells showed that metformin reversed silica-induced cell toxicity, oxidative stress, and epithelial-mesenchymal transition (EMT) in lung epithelial cells, and suppressed inflammatory response in macrophages.
EMT, a process by which epithelial cells gain migratory and invasive properties, plays a critical role in PF development.
The diabetic medicine also prevented TGF-beta 1-induced fibroblast maturation into myofibroblasts.
Simultaneous treatment with metformin and an AMPK blocker reversed metformin’s beneficial effects, highlighting their dependence on AMPK signaling.
Overall, these findings indicated that “metformin, dependent on AMPK signaling, attenuated silica-induced pulmonary fibrosis by decreasing cell toxicity, inflammation, oxidative stress, EMT, and fibroblast activation processes,” the researchers wrote.
As such, metformin “could be an effective therapy against silica-induced lung fibrosis in different stages of [fibrosis],” they added.
Because previous pharmacological studies suggest that metformin “is unlikely to reach the lung tissues with high concentrations” as an oral medicine, “metformin inhalation therapy may achieve better results in the future with fewer side effects,” the team wrote.