Making Tough Decisions as Pulmonary Fibrosis Progresses


This is a difficult blog to write
I’ve been making decisions about how to spend my limited time and energy wisely. I was hoping to bounce back after I experienced a decrease in lung function about two months ago. But a trip to my doctor caused me to face the fact that this is my new normal.
I have mixed feelings about adjusting to the new normal. On the one hand, facing up to it helps me assess what is real, and what I need to do to make wise decisions. On the other hand, I struggle with this process because of the grief I go through, which I wrote about recently in “The Healing Cycles of Grief.”
As I face my new normal, it is evident I can no longer do all the writing and online projects I love to do
Here is some of what I am juggling right now:
- Writing two blogs.
- Writing a book for terminally ill patients and their families about being caring and compassionate with themselves on this journey.
- Recording another CD of compassionate statements we should offer ourselves as we struggle with the challenges of life.
- Compiling notes from a lot of workshops I’ve given in the past 25 years to pass onto others.
- Spending time with family and friends.
- Making some end-of-life decisions while I’m thinking clearly and able to.
- Doing Facebook Live videos.
- And tons more on my list . . . .
Guess what? I can’t do all this, even though I want to
Here’s the thing: I no longer have the energy or stamina to do all I’d like. I tried to figure out which activities to keep and which ones to let go, but got confused weighing all the factors.
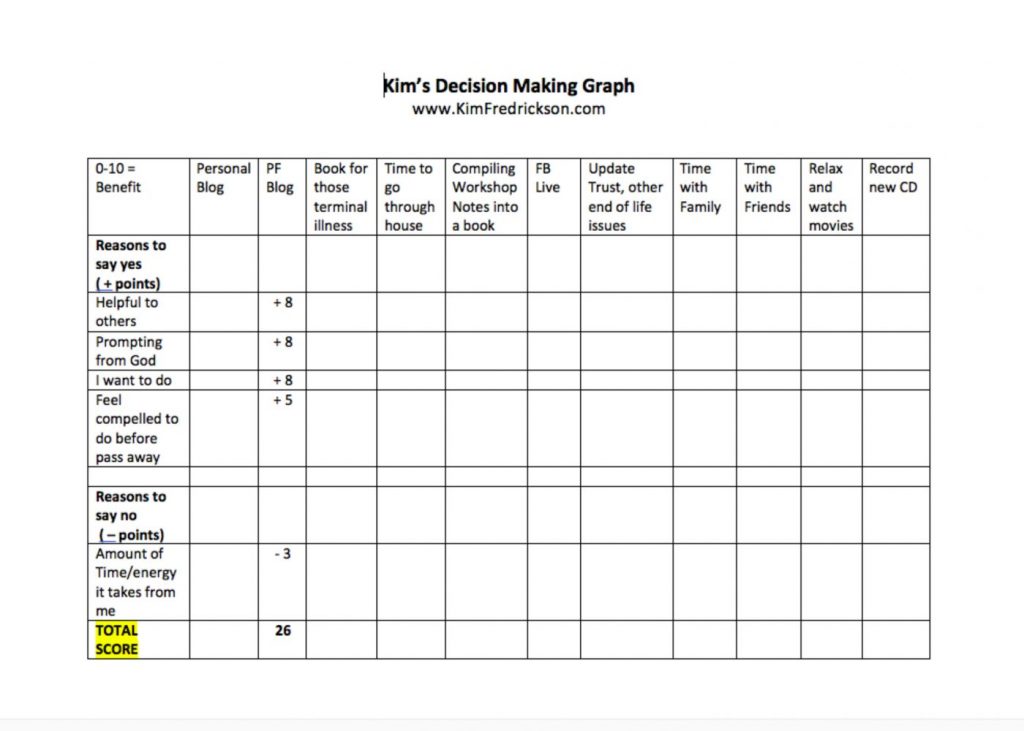
This may sound nerdy, but I needed to come up with a way to organize my thoughts and priorities. I created a chart so I could put everything in one place. On the top row, I listed each activity to consider, and created rows listing reasons to continue.
I gave points to each one (1 = not very important to 10 = very important). I then created a separate row to assess how much time and energy each item would cost me if I continued, and gave each a negative number.
I added all the + numbers, and subtracted the amount of time and energy each would take from me. Each category ended up with a final number. This chart helped me assess which activities to keep and which to let go.
Here is a sample chart, using this blog as one of the items to consider. I’m happy to say that continuing to write the blog is a priority. You can download a copy of the chart if you’d like.
I hope this is helpful. It is hard to face some of the decisions we need to make as our disease worsens.
For me it is important to think about the things I still want to do to have a positive impact on my world, as well as to have meaningful times with family and friends. It is also important to address end-of-life issues, taking care of details that need to be handled.
How about you? Do you have a way to assess how to spend the time you have left on what is really important to you? I’d love to hear your ideas and your process. And please share with others who might benefit by email or social media.
***
Note: Pulmonary Fibrosis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Pulmonary Fibrosis News, or its parent company, Bionews Services, and are intended to spark discussion about issues pertaining to pulmonary fibrosis.
Save
+++Save







Cheryl
This came at exactly the right time as my husband's IPF has taken a downturn and things are changing fast. He's been stable for almost 10 years so I think we got a little complacent. We are trying to figure out what to do next...from "do we get a stair chair and stay in our house" to "will he get another year to play a little golf?" I hate this disease!! Thank you for writing this blog...it helps a lot.
Kim Fredrickson
Hi Cheryl...thanks so much for your comment. I'm so glad he's been stable for so long. Those downturns are so hard, and require lots of adjustments. I'm so glad my blogpost came along a the right time, as you make wise choices for the future. I hate this disease too!
Chet Salisbury
Are you not a candidate for lung transplant ???
Kim Fredrickson
Hi Chet...I wish I was. My PF was caused by the chemotherapy and radiation for breast cancer. I'm not eligible to be put on the transplant list until I am 5 years past my treatment for cancer. I'm 3 years cancer free, and have to wait 2 more years to even be considered for the list, even though my PF is bad enough to get on the list now.
Laura Reed
Oh my ! I am so grateful for this blog and you and the comments- we don't know what to do- get a stairlift- move to a one story?( but we would have to sell first) how do you know when the end is coming? There doesn't seem to be answers. He is o2 full time and can't do our stairs- then he said yesterday if we stay I would like to die in the dining room so I can watch my birds... I lost it
Kim Fredrickson
Hi Laura,
I'm so glad my blog has been helpful, but so sorry you and your hubby need to be reading it. Your comment is such a good reminder of how much our loved ones suffer along with us. It is so hard to not have a lot of answers, and have so many important decisions to make. I can see how you "lost it" when your husband shared what he did. I have those kind of thoughts too about end of life decisions. i encourage you to take steps to do whatever you can to make your lives easy with a better quality of life. If getting a chair helps, try to do it. This would be way less stress than moving etc. I know these decisions are hard, and there is so much on your shoulders. Your hubby is so blessed to have you by his side.
Lauralee
I am slow to ask/say this.
I was told I am in denial or I am cold and selfish. *(52yrs old)
I have spent my entire adult life in surgical nursing.
NON smoker.
The mother of a PHH baby. ***(before PHH).
I now have PF, PHH, & TBM.
24/7 O2, Walker/Wheel chair. All diagnosed in the last 9 months. *(DNA)
I can rattle off a whole string of data, have my "arrangements made. I find myself at a loss.
I spent the past year reassuring the planet. I was fine, so I would not disrupt life for everyone else.
Now, I am not sure what I really feel. I am to exhausted to be angry. Hate whiners. So, I try not to whine. I don't have the skills to through myself a pity party. What's left?
I met Prince Charming, and 4 months later had "the cough".
We had survived 1.1/2 yrs.
He is better at this then I am.
I have not given up. I'm just a tad lost.
Please, jump right in.
I need honest feed back.
Thank you for the knowledge and compassion you share.
Kim Fredrickson
Hi Lauralee...I am so glad you shared what you are going through! I can't even imagine having to process SO MUCH in such a short period of time. It sounds like you handled a lot of stuff and took care of details, all while taking care of those around you who are being affected too.
And now...the disorientation, feeling lost and not knowing quite sure how you feel is catching up with you. Everyone goes through these stages of grief in our own way, and this is your way. Give yourself time to not know how you feel and to be a tad lost. That's ok. I love your question...what's left since being angry, being a whiner, or throwing a pity party doesn't suite you. I would recommend treating yourself with kindness and compassion right where you are. Do things that bring comfort, enjoy the things you can, and allow Prince Charming to care for you.
I'd also recommend talking to yourself kindly, maybe like this, "This is so hard, I've been through so much and don't know what I'm thinking or feeling half the time. That's ok...it's amazing I'm doing as well as I am. I have spent my life helping others through medical problems, and I am a fighter. One thing I know is I am not in denial or cold and selfish. I'm gifted to be able to handle reality and deal with "what is." Others may not understand, but I do. I'll put my efforts into being kind to myself and enjoying the life I have left."
I hope this is a help. My heart goes out to you fellow PF Warrior. I'm sending love and prayers your way...oh, and a hug too.
Laura Reed
I love you Kim and wish I knew you personally- I have said it before but it is a cruel, not well known about enough disease!thank you for you
Kim Fredrickson
Thanks Laura...sending you love too. I appreciate your encouragement. It blesses me to know that my efforts on this blog are helpful to you.
Roberta
I can't find where to leave a comment except after someone else, so I hope I'm not stepping on any toes doing it this way.
It's been a long journey to get where we are. My husband has cystic fibrosis, it was a long hard battle to get that under control and to get him used to med and treatments and everything else we needed to learn.
Aug 2016 an added journey path came when I was diagnosed with PF. Wow, to go in a matter of moments from no oxygen to constantly for oxygen 24/7, the labored breathing, this COUGH...it's been years for the cough.
I don't think I can ever get used to this life. I refuse to give in. No plans for the end, I've been doing research and I'm going to try and handle this holistically. I have nothing to lose, no cure, no real treatments. So that is my plan. Now I have to find the herbs I need. Some are difficult to come by. Wish me luck.
Kim Fredrickson
Hi Roberta,
Thank you so much for your comment. I'm sorry it was hard to figure out how to leave it. Wow...you have been handling so much as a couple dealing with your husband's CF, and then to have you diagnosed with PF too...I can't even imagine! It has been SO HARD for me to adjust to using O2 24/7 too. Everything does change in an moment. I love your attitude of refusing to give in, and doing research to explore all options. I wish you the very best of luck, best wishes, love, and great success! I also sent a prayer to God on your behalf. Many blessing my PF friend...
Aleatha
Is there a support group for PF. I know there is one for sarcoidosis. My daughter suffers from that. I have PF. Oxygen 24/7. Coughing every waking moment, spitting up mucus. I have blacked out a few times from coughing uncontrollably. My body is so tired. Trouble breathing makes me cough, itching throat makes me cough. Nothing seems to help. I feel like I'm living with this alone. Although I have a husband and two daughters. Depressed most of the time. I'm not on the list for transplant but they want to put me on after I lose some more weight.
Kim Fredrickson
Hi Aleatha...great question about support groups. I know there is one in my area. Check with your pulmonologist, and the nearest hospital that treat PF. They often have them. I'm so sorry you have so many awful symptoms...that sounds so miserable. You need someone to fight for you. It seems like there must be something they can give you to help with the cough, and your depression. Please consider getting a second opinion from another pulmonologist. Sometimes they have different ideas. My first pulmonologist gave up on me, and I switched and got better care. You are worth fighting for!!!
melanie mahler
I hate watching my 84 year old father suffering from this disease. A delayed diagnosis and even further delay with esbreit prescription has resulted in a downslide that seems to be neverending. My dad has now been referred for palliative care and it was hard enough for me to sit there in doctor office and hear the short time they suspect he has left, let alone for my dad to hear those words. My dad's weight is down to 154 pounds now - for a 6'2" man, it has been hard for him to maintain his weight despite meal replacement drinks, etc. He's so disappointed to see his weight slip again and again. This disease really sucks!
Kim Fredrickson
Oh Melanie...I'm so sorry for your Dad's decline and you having to watch him get worse. Being referred for palliative is so devastating, I'm so very sorry for both you and your Dad. Yes, this disease really does suck. I'm sending prayers, love and blessings your way.
Wendy Ford
I'm in a position where I am now on 12 litres of oxygen and since having a chest infection has really knocked me down.
I'm having a stair lift fitted, as my toilet is upstairs.
I have limited time out as liquid oxygen doesn't last so long and have 3 units.
I still drive and go out and about on my own.
I'm also listed for double lung transplant as 58 this year.
Had Ipf for coming on 6 years.
I'm getting worried now as know my time is limited.
Really worried about my husband and family as they are not coping well about my future.
Help
Kim Fredrickson
Dear Wendy, thanks so much for sharing your situation with us. You are an inspiration, taking advantage of every resource to help you stay as active as possible. I'm so glad you are getting a chair lift installed. That will make such a difference for you. Good news that you are on the transplant list, and are living life the best you can. I'm so sorry that you have to bear the burden of how your family is doing with your prognosis. I know it can be hard for family members to accept reality and work through their own feelings. I'm wondering if your pulmonologist could recommend a counselor to help your family deal with the reality of what is happening so the burden is not on you. Best Wishes to you, and thanks for being an inspiration to me.
Steve
Thank you for this blog. I am 62 and was diagnosed with Ipf over 7 years ago. I am so far very lucky. All I lacked in life was a grandchild and now we await the arrival next week. My prayers were answered.
This is a strange, confusing, horrible disease. No one seems to understand it; which makes coping a very lonely excercise.
But don't feel sorry for me yet. I have no outward symptoms outside of shortness of breath when I exert myself and declining PFT results. I know it's coming though so I am going to try to enjoy my life to the fullest, love my family and friends, plan ahead, keep busy, and try to be myself regardless of my disabilities.
Kim Fredrickson
Hi Steve, thanks so much for sharing with us. Congrats on your soon to arrive grandbaby! I'm so happy for you!!! I'm so glad that you do not have many symptoms yet that limit you. I love that you are living life to the fullest, and are enjoying your blessings. Keep it up...every moment is precious. Many blessings to you.
Jeffrey Carter
Steve, and Kim, I have a question... you, Steve, have lived for 7 years with IPF, I've lived for 3 and still in good shape, but I switched to the paleo diet soon after diagnosis and after some research, and the sense of 'hot' lungs I had disappeared, and so far so good... I feel pretty normal, but sometimes the cough attacks. In addition, I haven't had any colds, which is something that now scares me. Do you have any 'secrets' for the 7 years, or is this disease 100% unpredictable... Of course, I realize Ms. Fredrickson that Steve isn't in a conversation, so I wonder if you have any advice on that score... Just maybe Steve checks in... Jeff
Kim Fredrickson
Hi Jeffrey...so good to hear from you. Great to hear you are doing so well. I'm afraid I don't have answers to your questions. It seems like people progress at different rates. I progressed very quickly because my PF was from chemotherapy and radiation for breast cancer, which progresses quickly. I hope Steve checks in too. Best Wishes to you...
Janet Rose
I really need this blog right now as I have no one to talk with about my husband's PF. He's 70 and was initially diagnosed almost 2 years ago. Due to an incompetent pulmonologist, he has not been treated with medication for PF. THE PAST 2 months have been spent getting accurate diagnoses. He is about to begin treatment with an anti-fibrotic. He's on 02 (2.5-4 liters) 24/7. I appreciate reading the comments because it gives me some idea about what lies ahead.
Kim Fredrickson
Hi Janet...I'm so glad this blog is helpful to you at such a difficult time. Ugh, I'm so sorry your husband's diagnosis and treatment have been delayed due to incompetence. That is so awful. I hope the medication will be a help to slow down the progression of his PF. I'm so sorry for all the frustrations and fears you are going through as well. Your hubby is very blessed to have you by his side. My very best wishes to you both...
Karen Williamson
Hi I love this blog!! It is a comfort to know I'm not alone facing the exact same decisions. I had SCLC. Now I have severe COPD. I am going on 7 yrs cancer free. How would I get on a list for lung transplant? My Dr. once talked about removing the part of my lung that is no longer functional but now she has changed her mind and said it only has a 10 yrs survival rate. I feel like this 10 yrs is more then I might have without it. She won't do it. I'm 56 yrs old. Any advise would be wonderful. I use oxygen at night with my cpap machine. During the day when I need it. I'm not ready to go completely on oxygen yet. I sit here now sick. Thanks for letting me write.
Kim Fredrickson
Hi Karen...I'm so delighted to hear my blog is helpful. That's what I've been hoping!!! Oh my, you've already been through so much. I'm sure your doctor has good reasons, from her perspective, for not removing a part of your lung. I would ask her strongly for a referral to the closest hospital program to you who do lung transplants. If she isn't willing, I would consider getting a second opinion from a esteemed pulmonologist in your area, and see if that doctor will give you a referral. I know that to be considered you need to be considered "severe" and there are standards that determine the severity of your disease.
My first pulmonologist gave up on me, and wouldn't refer me, so I switched. My second one is very supportive and has referred me to UCSF for a second opinion and consideration for a lung transplant.
It is your life, and it sounds like you want to pursue every possibility. Be strong, ask for what you need...and the very best wishes to you!
Jeannine R
Go to unos.org and look up hospitals that do lung transplants and see which one is closest to you. Call them and set up the evaluation. That's what I did. I then requested my medical records to be sent. Good luck. Take charge of your situation.
Kim Fredrickson
Hi Jeannine...I love your wonderful and assertive self! I actually go to UCSF regularly (they do lung transplants), and they are the ones who say I have to wait two more years. My husband and I are thinking about investigating a transplant outside the US, which might have less strict standards having to wait 5 years to be cancer free. Good luck to you as well!
Patrick Cramblet
I have just been diagnosed with Pulmonary Fibrosis. Not idiopathic. I am 76. I feel that being 76,obese and type 2 diabetics that I would not be eligible. Don't know for sure. Right now I am on 2 liters going out and on 3 liters sleeping. Anybody know ground rules on lung transplants?
Kim Fredrickson
Hi Patrick, I'm so sorry you've been diagnosed with PF. I would check with your pulmonologist to see if you are eligible to be considered for a transplant. It's worth asking about! I know they take into consideration your overall health, weight, and the severity of your PF, as well as other things. You are worth finding out if that is a possibility for you!
Kristin
Kim, you are so amazing! My mom was diagnosed in 1985 at and she passed away in 1987 at 37 years young. I was only 11 when she was diagnosed but I remember her always keeping a smile on her face for me and my brother, even though I knew just getting us up and ready for school was exhausting for her. I admire everything you are doing. I wish my mom had all the support and blogs such as yours when she was suffering. It was preinterent. Thanks for this great read! Fight on lady warrior!!
Kim Fredrickson
Hello Kristin...thanks so much for your very encouraging response. I'm so sorry you lost your mom at such a young age :(
I'm so glad you have positive and loving memories of the sweet times you had together. I can't even imagine how hard that must have been for her to have so little information and support. I'm grateful to be able to blog about my experience living with PF, and I also receive such encouraging support from caring friends like you. Many blessings to you, and thanks for taking the time to encourage me!
Georgie Farris
Hi Kim just found you and have read some of the letters people have written in to you, I was born with a curve spine and very short in status. had surgery at age 11 had fuson put bone in spine to make it better for me to get about which I did grew into a woman worked kept house got married no children Back kept getting worse . to make a long story short my spine has now curved to the point
that it is pressing to my lungs I am on oxygen 14 7 to go out have to take portable oxygen so use the d tank and it is heavy to carry as I am so short . at home I get tangled up in the oxygen hose when walking thru the house what do you do about that bought a portable sweeper that has helped some. Like every one else you feel sorry for yourself at he begining then you pick yourself up and try to do what you did before this happened and you find out you can;t that is the hardest for me and on 2 liters of oxygen but can't be with out sleep with a bi pap as can;t eliminate the carbon dioxide any info will help in making life a little easier for me in the home enjoy this blog and wish you the best Georgie
Kim Fredrickson
Hi Georgie...I'm so glad to hear from you and learn about your story. You have been through so much!!! Somehow you keep going and adjust to the many ways your life has changed. Living life while using oxygen 24/7 is quite a challenge! I hate tripping on the cords too! It is hard to explain to others how tiring and complicated it is to go anywhere because of needing O2. Know that I understand. I'm so glad you found my blog, and I look forward to connecting with you again. Take Care...we're in this together :)
Esther Landers
Hi Kim it's me again . I love reading your blogs. My husband had colon cancer 10 years ago and chemo treatments. I am wondering if the chemo could have caused it as they diagnose him as ipf unknown cause. He never smoked. Dr never pursued the reasons is there any way to find out what caused it? Thanks again
Kim Fredrickson
Hi Esther...always good to hear from you. I'm not sure how to answer that question. You could do research online to see if the particular type of chemo your husband received also is known to cause PF. Also ask your doctor and bring in the research you found. My PF started immediately after finishing chemo and radiation for breast cancer, so that's why they knew what caused it. There is research that shows the specific type of chemo I received was linked to developing PF (only 1-2% chance). There is also some research that radiation, especially if near the lungs can cause it. It is so normal to what to know why your hubby got this disease.
Janet Rose
Radiation has a well known link as a cause of IPF.
Kim Fredrickson
Yes...so true Janet. Thanks for your comment.
Georgie Farris
Hi Kim first want to wish you and your Family a Happy Easter. Going thu daily chores with hose hanging out of your nose and hate looking in the mirror saw on your page yesterday about the glasses you can get now that you can connect your canula to the glasses called about them they are not cheap. Do you know any one has gotten them and are they happy with them let me know , Thanks and Hang in there we are all in this to gether
Kim Fredrickson
Hi Georgie! Happy Easter to you too! Regarding the glasses, no they aren't cheap, and they are only for those using 5 lpm or less. I actaully am talking about them as a part of next weeks column as I share about how my vision has changed over the last year. Those who I've talked to really like them. I wish I could. Yes....we'll hang in there together!