Measuring My Improvement in the Year After Transplant

I received my new lungs a year ago, on Aug. 14, 2020. Now it’s time for me to reflect on my quality of life.
Initially, I evaluated my progress by how long I stayed in the hospital. Unfortunately, I failed my goal to leave the hospital at the two-week mark because of health issues. This failure caused depression and concern. Then I learned to use my recovery issues, physical condition, and test results to monitor my progression.
First 45 days: The worst days
In the initial 45 days of my recovery, I saw minimal improvement in my breathing and physical condition. The slow progress kept me distressed. My health issues affected my physical condition and test results, so, I used them as my primary measurement.
I had three main wellness concerns. Firstly, I fainted on the first day of recovery, which led to two small tears in my incision. This haunted me. Because of the openings, I continued to have fluid around my lungs, and it kept them partially collapsed.
Also, the tears leaked a lot of liquid. I felt like Carrie in that movie based on Stephen King’s book of the same name. My hospital gown would be soaking wet, along with my chest and lower body.
Then, around Aug. 25, another complication arose. I thought I had a heart attack, which turned out to be atrial fibrillation. A few days later, I had a transesophageal echocardiogram with cardioversion to get my heart back into normal rhythm.
Another problem was that I had an additional surgery. My surgeon wanted to rough up my chest wall to help the lungs adhere better and to eliminate fluid and air. This procedure is called pleurodesis. Also, he talked about exploring the wound. These two surgeries were combined.
Having another surgery didn’t thrill me. On Sept. 3, I had the surgery, which eliminated all of my previous improvements and caused more pain and dizziness. The surgery also caused me to faint three times, and these falls contributed to my worst day of depression.
To check my physical recovery, I charted my speed on the treadmill. From Monday to Friday each week, I walked on the treadmill for 30 minutes. The following graph confirms how little progress I made.
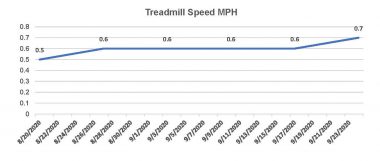
After transplant, Kevin tracked his recovery by tallying his treadmill speed. In the first 45 days, he didn’t see much progress. (Courtesy of Kevin Olson)
Exercise helped, but the overriding factors were my persistent health problems.
The next 135 days: Transition
On Sept. 28, I had a significant recovery breakthrough. A healthcare provider drained 800 cubic centimeters of fluid from around my left lung. It allowed me to breathe easier and eased my pain, which led to a transition from no improvement to speedy progress. Now I could measure my physical condition and lung function and get a meaningful picture.
With my health problems solved, I increased my treadmill speed exponentially, and my lung functions rapidly improved.
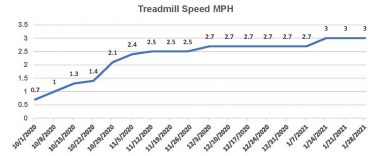
After draining fluid from around his lung, Kevin was able to improve his treadmill speeds in the second phase of post-transplant recovery. (Courtesy of Kevin Olson)
After the transplant, pulmonologists monitored my spirometry forced expiratory volume in one second (FEV1) to detect improvement, as seen below.
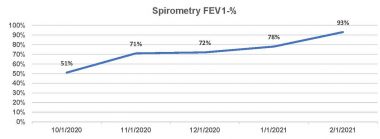
Kevin’s forced expiratory volume in one second chart is more proof of progress. (Courtesy of Kevin Olson)
Now, my worries about recovery were gone. In addition to the empirical data, I noticed a physical and emotional boost.
I had my best day on Oct. 9, when my wife and I went to a park for a walk and to enjoy the scenery. With lots of energy, I walked across a field. However, I had to be careful because of the holes and sticks.

On his best day post-transplant, Kevin went to a park and walked across this field on Oct. 9, 2020. (Courtesy of Kevin Olson)
Next, I had an emotional breakthrough when friends came to visit us, which bolstered my morale. During the visit, my U.S. Military Academy classmates said I needed to pay attention to detail and move my arms 9 inches to the front and 6 inches to the rear. This minor suggestion allowed me to regain my natural balance.
Last 6 months: Fantastic months
In the final six months, my FEV1 continued to rise and stay in the normal range of 80% and higher, as shown in the following graph.
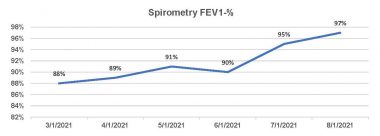
In the last six months of recovery, Kevin’s FEV1 results continued to rise and remain in the normal range of 80% and higher. (Courtesy of Kevin Olson)
At my six-month checkup on Feb. 3, my bronchoscopy showed no rejection or infection.
I finally realized that idiopathic pulmonary fibrosis (IPF) didn’t define me anymore. So, with the IPF barriers lifted, I started challenging myself.
- At the end of February, my wife, Dana, and I drove from Kansas City to Phoenix. My lungs were tested at 7,500 feet, and they passed with flying colors.
- I used stairs whenever possible, which led me to complete the American Lung Association’s Fight for Air Climb.
At my one-year checkup, I did a Snoopy dance. I still had no rejection, which means fewer appointments and labs in the future.
As I’ve shown, my quality of life has improved because of my donor’s lungs. Therefore, I consider Aug. 14 as a celebration of life for my donor. I am indebted to him for his unselfishness.
I am amazed at how much my quality of life has improved in a year. I am looking forward to more challenges, such as flying, in the second year.
***
Note: Pulmonary Fibrosis News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Pulmonary Fibrosis News or its parent company, Bionews, and are intended to spark discussion about issues pertaining to pulmonary fibrosis.









Leave a comment
Fill in the required fields to post. Your email address will not be published.