Pulmonary Fibrosis News Forums › Forums › Healthcare Questions › Diagnosis Information and General Questions › The Relationship Between PAH & Pulmonary Fibrosis
-
The Relationship Between PAH & Pulmonary Fibrosis
Posted by Charlene on May 10, 2019 at 8:37 am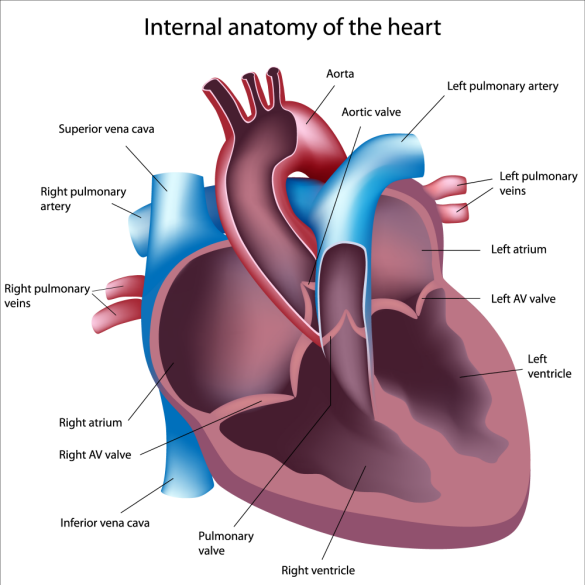
Photo did not originate from PF News, the original source can be found HERE.
While more and more research is being conducted about pulmonary fibrosis (PF) on an annual basis; there still remains a lot that is unknown about this life-threatening lung disease. As an example, sometimes PF develops as a result of toxic or hazardous exposure to chemicals, particles or other airborne issues, including pollen and environmental triggers. That said, oftentimes PF develops simply as “idiopathic” which is just a fancy way of physicians saying they don’t know what caused the lung disease. IPF is what I was diagnosed with a little over three years ago, and to my knowledge: there is no known reason why I developed this lung disease as such a young age.
Additionally, I’ve heard that PF can develop as a secondary disease following treatment of another chronic illness. As an example, I know a few people on these forums or throughout my own “PF community” who have developed this disease as a result of their therapies for cancer. This seems incredibly unfair, but sadly, it is a pretty common occurrence.
I recently saw a post on Inspire Pulmonary Media about pulmonary hypertension and it grabbed my eye, because the post was called Do I or Don’t I Have Pulmonary Hypertension?
I’ve been told that I have PAH as a secondary disease caused by my IPF. Simply put: my heart is over-compensating for my poor lung function. What is interesting is that one physician has told me I do have it, whereas others have told me I am just at risk for it. This is why the above article caught my eye! Sadly, I’ve had many friends die from PAH, including a very close friend back in September, Serena. Admittedly, it scares me that I may have or develop this disease!
I was curious about others’ experience with both PAH and IPF/other ILDs: have you ever been told you have Pulmonary Hypertension or are at increased risk of developing it?
Charlene replied 5 years, 5 months ago 10 Members · 22 Replies -
22 Replies
-
Hi Charlene,
Last week I got admitted into hospital due severe cough, cold and tightness in chest. I have had these things many times but I ignored them and was pushing myself to work. I was not on oxygen either.
at the hospital it was found that I got PAH ( RVSP. -38), high BP which is caused LVH on the heart along with Rhinosinusitis. Now I am on O2. I think its my fault that I pushed myself too far even with breathlessness.
Had I listened to what my body was saying I wouldn’t have had PAH. But it is what it is. One day or the other IPF brings other complications. Quality of life gets a hit when IPF is compounded by PAH.
-
Hi Moses,
Thanks for writing and contributing to this topic thread, although so sorry to hear of your recent admission due to a severe cough and cold. I always try to advocate how serious the ‘common’ cold can be for those of us with a lung disease to catch, but no one seems to understand entirely except this group.
Pushing through the symptoms is so common, but you’re right, it is likely so bad for our bodies. However, I am guilty of doing the same and know extra stress is being put on my heart. So sorry to hear that you now have developed PAH as well. Are they giving you any treatment to help manage the disease or symptoms? I sure agree with you about quality of life! Hang in there, and feel free to write anytime…
regards,
Charlene. -
Hello Charlene. I was diagnosed with pulmonary fibrosis seven years ago and with pulmonary hypertension 2 1/2 years ago. I was hospitalized on February 14 because of my breathing. I too am on 02. I used the 02 until about 2 months ago, doing well. This past Sunday it was so hot in the church that I could barely breathe. I went to my doctor yesterday and he wanted to put me back in the hospital. I begged not to go and he finally agreed. However, I must stay on my 02 and once again on massive dosages of Prednisone. He said I was in the beginning stage of relapse. I hate that it happened, but glad that it got caught before the full-blown relapse. When I was diagnosed after having a lung biopsy, I did not know what it was. The doctor at that time did not know that much either, he asked me to read about it on the internet. I have since changed doctors, excellent and very thorough. I get frustrated sometimes because he is through, he leaves no stone unturned. He knows my story. I pray we all does well with the ailment. I have good insurance that pays 100% for everything except medicine. I NEED help. Do you are anyone else knows where to go to get help for medicine? I have used Needymeds but………Thanks for listening. Marcia Jones
-
Hi Marcia,
Thanks for writing to us regarding this topic, but so sorry you’re also facing this cruel disease alongside pulmonary hypertension. Did your doctor ever link the PF development as a result of the PH? I’m always curious to hear of anyone who has a doctor that has linked the two with certainty as there seems to be some confusion around this.
The humidity really bothers me as well, sorry to hear of your struggle at church this past Sunday. Do you have any type of flare up causing the need for excess Prednisone and more oxygen/shortness of breath? Does he mean an exacerbation?
Hang in there and I hope you recover as soon as possible!
There are some agencies out there to help cover medication costs if you are in the US. Is that where you’re located? Which drug are you on – Ofev or Esbriet? I’d start with calling the makers of the drugs, which you can find online (Genetech produces Esbriet and IB produces Ofev) and ask about financial assistance for these drugs. Otherwise – do any forum members remember the companies assisting patients with finances off the top of their head?
Thanks for writing Marcia, feel free to connect anytime!
Charlene.
-
-
-
Hi Charlene,
I didn’t have an echocardiogram done till a year after the IPF was found on my chest x-ray (May 2013). And I’m not sure how long I had the IPF before that chest x-ray. My echo done in the spring of 2014 showed I had a mean arterial pressure of 28-30. But my pulmonary doctor was not concerned, he felt we could keep an eye on it. I was also on Bipap at this time for sleep apnea.
I was taken off Bipap in March 2018. (Long story) I had another echo May 2018. And my mean arterial pressure was down to normal, 16. My cardiologist was surprised. We’re not sure why it went down. Was it because of being on Bipap for 8 years??
My cardiologist will repeat my echo next spring, unless I have any new symptoms. Since diagnosed with the IPF, I have PAH in the back of my mind as my dad had pulmonary hypertension due to long term heart disease.
By the way, the ILD Clinic at UCLA pushed my appointment back until the end of June. I was disappointed, but there’s been no changes for me, so that’s okay!
Rose -
Hi Rose,
Thanks so much for writing and sharing a bit of your experience with PAH and PF. I find it amazing (not in a good way, though) how our hearts can suffer damage when our lungs are functioning poorly. I guess it makes sense that they have to compensate for an organ that isn’t working well but this seems really unfair; that poor lungs lead to a bad heart and likely vice versa. Ah well, so much about this disease is unfair I suppose…
That would be my (completely uneducated) guess re: the bi-pap helping to bring your pressures down. Glad they will test again, and I hope you remain completely symptom free 🙂
Goodluck with your appointment at the ILD clinic in UCLA. They do great work! I can understand your disappointment for sure, although June will be here before we know it.
Warm regards,
Charlene. -
Hi Charlene,
Thank you for the great diagram and insights about PAH. Even though I am taking supplements, laser treatment, and soon starting Wei Institute’s elixir (tonight when it arrives), I know PAH will remain a primary concern. My heart in the AM when I get out of bed jumps up to a little over 105 BPM but settles down quickly – less than 30 seconds and my O2 at those times is usually 97-98.
So it confuses me that the heart does that but also I have had an arrhythmia for decades and sometimes it can go into hyperdrive. Hopefully, a lot of this will go away when I am back home next week after a 14-month absence and the incredible amount of things we have had to work through (not the least of which was the “official” sentence of IPF), losing weight (automatically in the Philippines), and starting the aforementioned elixir. Truthfully though, I would rather have a heart attack than put my family through the usual end time suffering this disease causes.
No matter what, I’m going home. Now that’s exciting!… – Steve
-
Hi Steve,
Oh my gosh, I was so happy to hear from you yesterday morning! I was going to send you an email and just check in on how things were going. Thanks for writing 🙂
I didn’t know you’d decided to try out a blend from Wei, I think that is the same mix of herbs that Denny had much success with. Did the first couple nights with it go okay? Glad when your heart rate climbs in the morning, it jumps down rather quickly. Do you notice a significant difference in your HR at the gym, including how long it takes for it to come back down to normal rhythms? I really hope you see a reduction or a complete cease in the arrithymias when you return home. That is so exciting that it is getting closer! You must be thrilled? 🙂
Hang in there, it is so soon!
Charlene.
-
-
Thank you Charlene Marshall for all the information on IPF. I am going crazy and sad the we developed this no cure disease. I been on OFEV for 2? Years with no progression. My CT Scan is due on Monday then I will know If there is any changes.
What do you think about the herbal products .
Thank you
Karmin-
Hi Karmin,
Thanks so much for joining the PF forums! I’m glad you’re here and although I wish it wasn’t this cruel disease that linked us all together; everyone on these forums are so helpful and supportive. No doubt you will feel connected here. How did your CT scan on Monday go, do you have any results yet? How have you been tolerating the Ofev? Sorry for all the questions!
In terms of herbal products, are you meaning the Wei Laboratories ones? I haven’t tried them although some members of the forums talk about them in great success. I see Steve replied to you below, or are you talking about the Serrapeptase? Let me know and I’ll see if we can help 🙂
Cheers,
Charlene. -
@charlene-marshall
Hi Charlene – Yes I was glad to see your PAH post and for a while thought I had not been receiving any updates and was going to email you, too.
I had been considering Wei for a while since I could not find a laser in the Philippines. I started it Tuesday evening but no side effects or any differences are noted. It is the same recipe for all lung ailments we have and consists of pills that are called Soup A, Soup B, LC Balancer. I take two each 3x daily. So 18 pills more per day (yikes) but I probably only need to take it for two months and then go on a maintenance schedule (undetermined yet). They ship to the Philippines and it does not cost much considering the distance and only takes 6 – 10 days.
At the gym, I start with the recumbent bike and did 3.1 miles in 15 minutes yesterday. HR only went to 112. When I start working with weights rate does go up and stays there until I rest and I never wait long enough for HR to fully recover. Oddly enough that and the next day my O2 sustains at 96-98 mostly, same for laser treatments. So the mild to moderate workouts are a great benefit but so is packing my last two boxes with my airline tickets in hand!!! (Ooppsss – my HR just jumped…)
Had the director of the missionary training school we went to in 2016 (Philippines) looking for a laser too (he is an RN). You know I have a strong belief in our Creator so this next story amazes me. In that school, we had to participate in a live 40-day seminar (plus all other duties) and nightly there would be a health nugget spotlight. I talked to one doctor who gave it frequently not knowing her specialty. After graduating in December 2016, the director, his wife, me and my wife went to her house for dinner (her husband is a pastor), I thought nothing of it. Just a few weeks ago when I asked my friend to search for a laser, he asked if I remembered the doctor, of course, I did. Well, he reached out to her because she is a Pulmonologist. So, in other words, I met the doctor I need 2.5 years before I knew I needed her. Pretty cool, huh? – We meet on Facebook soon…
Any word or ideas regards an IPF get together?
Talk soon and stay well… – Steve
-
Hi Steve,
So nice to hear from you as always! The only “bad” part of these forums is how much we begin to care for others on here, and then when they aren’t active, we tend to worry a bit given the serious nature of our illness. I was very glad to hear from you the other day 🙂
It is a long weekend here in Canada, so I am just wrapping up a few emails and forum replies, then will be heading to spend the weekend with my family at the cottage. The first long weekend of the summer is always exciting here. Are you in the throws of packing/organizing this weekend? I’m sure you still have lots to do…
That is really great about the Wei products going to the Philippines, along with not being too pricey or long for shipping. Still haven’t been able to find a laser provider there? I hope the Wei products continue to not have any side effects for you. I’ll keep my fingers crossed you notice a difference like Denny did. I know he speaks so highly of their products.
I am so impressed at your commitment to be in the gym, despite the difficulties with IPF. Will you keep up the routine when you get back home? I know naturally you eat and live better there so maybe you won’t need a gym regimen/work out?
Your story about the Pulmonologist and meeting her long before you needed her gave me goosebumps! The world sure works in mysterious ways. I am thrilled you’ll be able to have her support when you get back home, that is wonderful. Will she be your primary physician do you think then, for the IPF?
No update yet on the IPF get together. I haven’t given it as much thought as I’d like as other things have been occupying my mind, it is on the list though!
Chat with you soon,
Charlene.
-
-
-
@Karmin-Chowbay
Hi Karmin,
If you are asking about Wei Institute’s elixirs, I am starting them tonight because I cannot find a k-laser in the Philippines where I am moving. If you want I can post again in a few weeks but it may take up to two months before it stops the IPF – if it works.
Stay well,
Steve
-
@charlene-Marshall
Hi Charlene,
Thank you for checking in. I was worried for you also the last week or 10 days and thought maybe I wasn’t getting updates too. I think sometimes no or less forum activity may be a good indication (I hope). But I know how busy you are so I just waited.
“Spending the weekend at the family cottage” conjures up ideas of fun and heat in the sun close to the ocean. – Hope it is both of those for you. Packing and final preparations are going well. There are times I don’t want to do this and could just abandon all my stuff because who knows if I will ever see it again… Not being morbid just know how much paperwork we have yet to do and nothing happens fast in the Philippines. So today (Saturday) I am relaxing until late and then do about an hour or so of stuff, make a final run to the store, and attempt again to figure out my suitcases. – Seems I’m taking a lot more pills than clothes this time. LOL. Sunday – my final day in this place is making some airline calls, fix pills for the next 4 days, do laundry after I shower, take the bed apart, bag up the remaining clothes and sofa cushions, and pack those final two boxes!!!
Wei seems to be going well but it has only been 4 full days. There is no class 4 laser over there and even the pulmonologist (we talked a couple of days ago) said she had not heard of one. She is looking for a doctor close to me as Manila (her home) is about 500 kilometers away and the only way to get there is to fly unless I take a series of ferries for about a week – nope… She is also looking for O2 there and says they do have that. I have a son who works for a medical supplier and visits lots of hospitals so I will see what he can uncover too.
I like the gym because it has a bunch of resistance/weight machines that have become a routine. Over there I will have to improvise but hope to get a new routine going. There is one gym not far from me there but they are not like the gyms here. The great discovery is how a mild workout stimulates mitochondria and raises O2 for a couple of days. So maybe the perfect remedy for IPF is gym, serrapeptase/nattokinase, laser, Soup A/B & LC Balancer. – Take that western medicine…
Stay well – Steve
-
-
Hi, Charlene,
First of all, I’m very sorry to hear that you’ve developed PAH as a result of IPF. From my own experience, I find that it’s emotionally pretty challenging to hear yet another diagnosis on top of the first one. Each time that happens for me, I have to find my way through on so many levels, and it’s not easy.
I, too, have developed PH, though mine is secondary to fibrotic chronic hypersensitivity pneumonitis, one of the ILDs. I’ve been having annual echos since 2015, and unfortunately the PH is progressing as the cHP progresses. As of yesterday, it’s been recommended by the team at my pulmonary clinic that I would have a right-heart catheterization to get a more accurate read of the pressures in my heart, as the pressures from the echo are only estimates. I’m not sure whether I will choose to have that procedure or not. To be honest, I am reaching a point where I am getting really worn out with procedures and all that comes with them: concerns about risks from the procedure itself and then the need for more appts and more evaluations to decide what the response should be to the results that are found during the procedure! After 7 years of managing this illness, it does all get a bit wearing.
I did want to mention that, just a few days ago, I watched a half hour FB Live presentation from National Jewish Health that was originally titled something like ‘SOB and Pulmonary Hypertension’. If you go to their FB page and scroll down to May 8, you should still be able to watch it. You might find it helpful, tho’ they didn’t talk much about SOB. Here’s a link to the page: https://www.facebook.com/NJHealth/Wishing you all the best,
Kate
-
Hi Kate,
Thank you so much for writing and sharing a bit about your experience with PH in addition to cHP. Like you, I struggle with any type of new diagnosis or even aliment since my IPF diagnosis; just seems unfair, doesn’t it? I hope you’re finding ways to cope with that and have lots of people surrounding you for support.
I hear what you’re saying about the procedural risks, complications, etc. when it comes to various diagnostic testing and monitoring. It is exhausting! I have had a right heart catheterization, and connected with a close friend ahead of getting mine done. I want to be honest, they aren’t pleasant but they are tolerable. The other good thing with this procedure is that it is usually only done once, so that was my approach: “just get it over with” type of attitude, but I certainly respect that isn’t for everyone. Feel free to connect anytime if I can be of any assistance in your decision making. It is tough stuff, for sure.
Thanks for the FB live link as well, I’m definitely going to bookmark it and go back and have a watch. I appreciate you passing it along 🙂
Wishing you well.
Charlene. -
Up till a year or so ago I didn’t have PAH…was diagnosed with IPF in 2013…and my FNP used to say she was glad I didn’t have PAH. Well now I do and I still don’t understand the ramifications. I’m a retired RN and should know better but sadly I don’t.
-
Hi Anne,
Thanks for writing, although sorry to hear you are now dealing with PAH in addition to IPF. This is something I struggle to understand thoroughly as well unfortunately, despite the explanations from my physicians. Would you FNP take the time to explain it and the ramifications of having both? Definitely ask them lots of questions! Take care, and feel free to write us any time.
Charlene. -
There seems to be different opinions in the medical field. I watched the videos from the PFF sumit and they talked about not letting sats and HR fluctuate too much as it can lead to PAH. Last week I had my first appointment at a Large centre ILD clinic. Upon going there all i knew was I had radiation induced PF but mild yet I have a lot of symptoms. First I had PFTs which showed a decline in lung function but remains in the mild disease state. Then the first doctor I saw asked me a lot of questions, examined my old CT (from April 2019 before I had symptoms other that occasional cough). He listened to my chest and stated I had crackles. He told us he thought I had IPF, in both lungs, likely brought on by the radiation. He did state it was mild but that the CT was old and very poor quality. He then left to go consult with the department head. The head guy came in and said “I am not convinced” he said that the fibrosis is so minor that it should not cause symptoms. He also said the crackles (Velcro sound) were very few. He states he is perplexed. I told him about the sat fluctuations, he told me to throw my monitor away, he does not believe in home monitoring. Rest when you get SOB he said. He then said PAH is rare even people with IPF rarely get it so it is not a concern. He told me so many things that were the opposite of what i have heard before, even from his fellow only minutes before. He said maybe that has caused me to have some anxiety ( ugh, I don’t). Anyway the CT was old and bad quality and not a high resolution so he said he is scraping everything and starting over, so i have no diagnosis at this time. He did a ton of blood work which definitely showed hypoxic lung disease but I have not heard what they plan to do about it. When I called to clinic to see if he saw the results they said no and he is gone on vacation lol. I said well have someone have a look. What a roller coaster ride. One good thing is i feel better mentally in that even though i get SOB easy i am not as worried about it, i just stop and rest. I have not checked my sat in a 4 days :). So for the long story.
-
Hi Nan,
Thanks for writing and sharing this experience with us. I know the center and the doctor you’re referring to (he isn’t mine, but I know who he is) and I am a bit disappointed in what-seems-to-be his lack of empathy for you and your symptoms. Yes the tests may not have shown severe disease, but regardless, your symptoms are hard to deal with. Being SOB can be so scary! I am also disappointed in hearing what he said about the oximeter. While I do understand (as I mentioned in my direct message back to you) the quality isn’t comparable to hospital-based measurements, sometimes seeing our values can put our minds at ease. See how it goes not checking in for awhile as he suggested, but please don’t feel you were wrong in doing so.
Unfortunately yes you are right about the medical field being seemingly mixed about the relationship between IPF and PAH. I wouldn’t go as far as Dr. S did about it being “rare” just based on the experiences from patients I’ve heard, as I am not an MD and have no medical training. However, being diagnosed with IPF is “rare” too when we all know it isn’t. I hope the new round of testing at least reveals some answers for you to start knowing what you’re dealing with. Keep us posted on how you’re doing!
Char. -
Dear Charlene and Dianne Jones,
You asked about how to get help to pay for medicines. I was put in touch with Healthwell. I am on Esbriet and Genentech might be able to help you there. I also was recently told by a nurse that if you just Google the name of the medication and “patient assistance” you can find help that way. There are many sources out there. I wish you luck in finding someone because these things are certainly high-dollar drugs. Karen
-
Thanks so much for sharing Karen!
I am lucky with having Canadian healthcare coverage, that I don’t pay a lot for Ofev right now and usually my employee benefits pick up the difference. I can’t imagine being forced to pay a lot of money for drugs we require to survive. Googling the drug name and then “patient assistance” is a great idea – I hope others use this tip!Unfortunately, last I checked, Healthwell is out of funding as they’ve used it all to help asking for financial assistance. Perhaps their funding has been renewed? I hope folks check it out.
Char.
Log in to reply.
