
John Oman
Forum Replies Created
-
John Oman
MemberFebruary 3, 2022 at 2:54 pm in reply to: Possible Cause of IPF – Ammonia ingestion and Statin?? Progressive?Hi! First, I’m not a Dr. and don’t play one on TV. I’m just another IPF patient. I assume you have IPF and the “I” stands for Idiopathic and the meaning is that the cause of the PF is not known. So, is it progressive? The answer is yes, unfortunately. If the cause were known and an autoimmune issue, I know of many that have been virtually stable for years. Otherwise, I’m afraid progression is what we have to live with. OFEV and Esbriet are the only FDA approved drugs for IPF and the data is overwhelming that the do help to slow the progression. It’s almost certain that if you don’t take one of them, your progression is going to be faster. Therefore, we really don’t have any choice. It is also not a certainty that you are going to experience serious side effects or that they cannot be managed satisfactorily. My suggestion would be for you to give one of them a try and if you develop unmanageable side effects, try the other and don’t worry about a side effect problem before it exists. Good luck to you!
-
Does your dad use a cannula or wear a mask like device over the nose? If a cannula, I’d suggest trying a mask. I can imagine that having that much oxygen jetted directly into the nose could cause excessive and unnecessary nasal tissue irritation.
-
John Oman
MemberOctober 19, 2021 at 2:51 pm in reply to: Post-nasal Drip: Another Ailment to Deal WithI too have an intermittently running faucet for a nose and a chronic problem with bronchial phlegm/mucus that has me frequently coughing and clearing my throat. “I” believe this is due to damage done by a decades long bacterial infection that “I” believe was also an underlying cause off my IPF. If and when it becomes available, I’m hopeful that N115 / sodium pyruvate nasal spray will be helpful.
-
N115 / Sodium pyruvate nasal spray. I’m not a Dr. and do not play one on TV. I’m just an IPF patient with limited treatment options like the rest of you. I too find the last phase III trial intriguing. I have not been able to find the nasal spray on the market with or without a prescription. However, sodium pyruvate is available in powder form from a number of sources. I’m considering purchasing the powder form and making my own nasal spray based upon dosage described in the past phase III study. I plan to discus the idea with my pulmonologist on my next visit.
-
Allan,
Again, I’m not a Dr. and have no medical training of any kind. Consider the source.
Phlegm with yellow color… When I had the bacterial lung infections, yellow was the color of the thicker, tacky phlegm that I could, sometimes, get coughed up from the lungs. Sputum culture of this phlegm yielded the bacterial infection, heavy infestation lab test results.
Sometimes… Getting good sputum samples from deep in the lungs is difficult to do. Samples are almost always contaminated by the plethora of normal oral, nasal, sinus, throat, upper airway stuff that can mask what little target phlegm we are trying to get evaluated. I had several ‘negative’ results before finally getting ‘positive – heavy infestation’ results. A credentialed respiratory therapist cousin of mine confirms this difficulty. There are complicated clinical procedures involving putting vacuum suction tubes down into lungs to collect samples.
Here’s what I learned and did… I never knew when I was going to be able to get up a ‘good’ uncontaminated sample. So I kept a few sample cups around and ready, particularly at night, ready for morning clearing coughs. When I sensed that what I coughed up was thicker, tackier and with little contamination, I spit it in the cup and sealed it up. I don’t think a large sample is required and I didn’t try to double up samples in a cup. If it was going to be more than a couple hours before the sample could get to the lab, I put the cup, in its plastic bag, in another container with ice cubes to keep it cool.
I did a web search this AM on phlegm and found the following link interesting…
Phlegm: Colors, textures, and home care (medicalnewstoday.com)
I’m rooting for you!
-
I’m in the same situation as Bob. No IPF cough. Frequently, not always, early morning cough to clear mouth and throat. I’d sure like to figure out what’s different about the mornings that I don’t have problem. So far I have no clue.
-
I’ve got it too… But assumed it was from old age and depravity…
-
Inogen TAV (Tidal Assist Ventilator): This is a relatively new product and I believe I am one of the first to buy and use it. It functions as both a conserver and to provide ‘tidal assist’. It works with gaseous O2 tanks or Inogen’s special model concentrator that delivers the higher pressure (50psi) needed by the TAV. There is a full description of it here: https://www.inogen.com/blog/what-is-tav/
I do not need/use supplemental O2 for leisurely activities but beyond that, doing physical work, walking fast, climbing hills/stairs, etc. I need much more than portable POCs can provide. So I use a small gaseous O2 tank, an MB08, 228 liter, 3,000psi tank weighing 2.3lbs, 3.2″ diameter, 11.8″ height. I put the tank in a small back pack with chest strap (and belly strap too but I don’t often use it). I find the TAV performs as advertised. I have tried a number of conserving regulators including smart/electronic ones and find the TAV much superior, both better at conserving and the tidal assist reduces the effort required to do rapid, deep inhales. With the TAV in a pocket or worn as a pendant around the neck, I particularly appreciate the ability to quickly and easily adjust the bolus size/duration with a simple press of an increase or decrease button as my exertion level increases/decreases. No need to get the tank into your hands and look at the regulator settings to do this.
That is not to say that it’s a perfect system. It is not. First off, it is expensive. Just under $1,500 if I recall correctly. There are two hoses to the TAV pendant/hand unit, a heavy O2 supply line to the tank/regulator and a normal cannula hose and they complicate the donning of the gear. It uses a special, venturi effect cannula they call a pillow cannula. It’s made of soft silicon rubber designed to seal in/against each nostril. It requires a little practice and fussing to get them in place correctly. I’ve not worn it for more than an hour at a time and I don’t now if the pillow cannula will become bothersome when worn for long periods. It is also noisy. There are venturi jets within the cannula jetting O2 at much higher velocity than normal systems. Those near you are definitely going to hear it, especially at the higher settings.
I’ve already suggested to them that they build the electronic/mechanical part of the TAV unit into the regulator on the tank. Then only one hose is needed, the cannula run from there. A hand held / pendant remote control could then communicate via Blue Tooth (BLE) to control the TAV hardware at the tank.
-
Conservation of the oxygen supply: As has been discussed above, the pulse modes of the POCs are designed to help conserve their output O2 and deliver it more timely/effectively to the patient. Another method of conservation is to add an O2 reservoir at/near the cannula to store the O2 from the concentrator during the patient’s exhalation and delivering it to the patient during their inhale. A study on the topic is available at NIH https://pubmed.ncbi.nlm.nih.gov/3931988/
Several products are on the market with names such as Oxymizer and Oxysaver,
-
Liquid Oxygen (LOX) home and portable systems can deliver significantly higher flow rates than concentrators and have light weight portable sizes that can deliver high flow rates for significantly longer periods than portable concentrators or gaseous oxygen tanks. However, they are expensive, not widely available and not reimbursable by most medical insurance plans or Medicare. The high density of cryogenic liquid O2 and the need to continuously vent gaseous O2 to cool the cryogenic liquid poses significantly higher storage, transportation and point of use ventilation requirements/regulations and fire/safety risks than gaseous O2 systems. As with gaseous O2 systems, they cannot be taken on board aircraft.
-
This is information that I’ve collected and tabulated myself doing web searches. I have IPF and use supplemental O2, up to 8 liters per minute (lpm) for more than leisurely activities. I am also and engineer and am working with a group at Johns Hopkins to develop more effective supplemental oxygen systems.
 :
: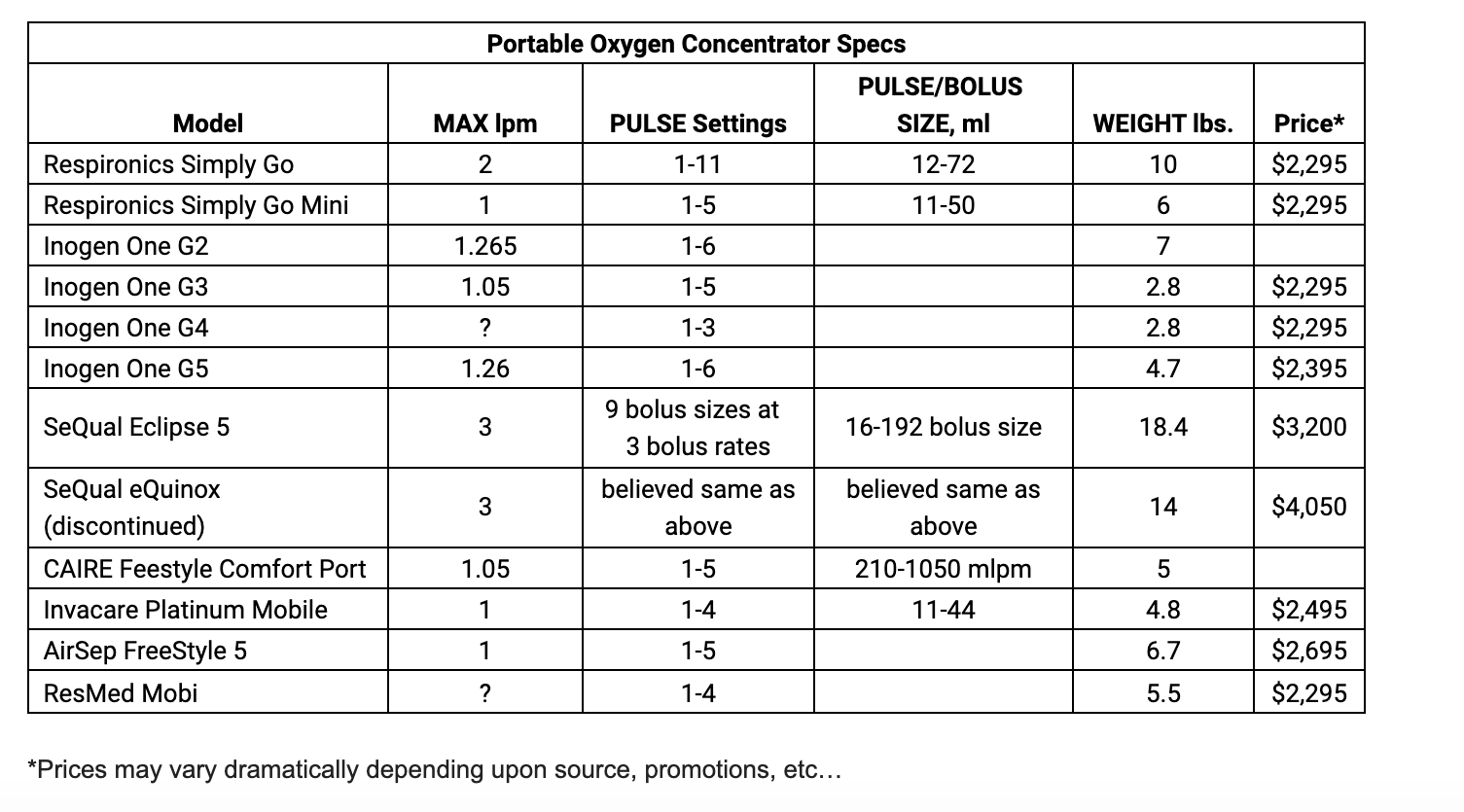
NOTE: PULSE settings CANNOT be directly equated to continuous liter per minute settings. It’s more complicated than that. A simplified example…
If your system is continuously delivering you O2 at a rate of one lpm into your cannula and you are inhaling half the time and exhaling the other half, then one half of the O2 is being wasted because you are exhaling against it while its being delivered. However, if your delivery system could, instead, squeeze all of its one lpm capability into/during the time you are inhaling, you are getting twice as much O2, effectively two lpm during inhale when you need and can use it. This is what pulse modes are intended to do.
That was a simplified example. It is more complicated than that. Typically you are not inhaling half the time. Also, towards the end of your inhale cycle, some of the O2 is not in your lungs long enough for effective transfer to your blood and some of it never makes it past your upper airways before it is exhaled out and thus wasted. Systems that deliver more of their O2 early in the inhale cycle can provide for higher, effective delivery rates to the patient.
In my view, a POC at its highest pulse mode setting can, AT BEST, only provide you, in effect, with up to three times its continuous flow rating. Most will fall well short of that.
-
Prices were approximate about 6 months ago.
Best source of information I’ve found (though they are selling them) is: Oxygen Concentrator Store: Oxygen Suppliers for Oxygen Equipment
-
Data I collected a few months ago. Prices were approximate at the time…
-
https://www.oxygenconcentratorstore.com/ is one of the best sources of information that I know of. Of course they are trying to get you to buy as well.
Here’s some data I gathered some months ago…
Portable Oxygen Concentrator Specs
Respironics Simply Go
Respironics Simply Go Mini
Inogen One G2
Inogen One G3
Inogen One G4
Inogen One G5
SeQual Eclipse 5
SeQual eQuinox (discontinued): believed same as above
CAIRE Feestyle Comfort Port
Invacare Platinum Mobile
AirSep FreeStyle 5
ResMed Mobi -
First a disclaimer: I’m not a doctor and I have not played one on TV…
I have, for decades in the past, suffered from massive night sweats. Also decades ago, complaining of chronic productive cough, I was diagnosed with chronic bronchitis probably as the result of previously being a heavy smoker. I was told there was nothing they could do about it, given prescriptions for Advair and albuterol and told to deal with it as best I could.
I was diagnosed with IPF one year ago. Several months ago, learning that a productive cough was not normally considered a symptom of IPF, I insisted we try to figure out the underlying cause of the productive cough was. A sputum culture indicated a bacterial infection. An antibiotic was prescribed and the productive cough, the night sweats and some other symptoms waned. However, a month later and my earlier symptoms began to return. A subsequent sputum culture indicated heavy growth of a different bacteria – Moraxella catarrhalis. I’m just completing two back to back prescriptions of azithromycin. 25+ years of chronic bronchitis, chronic productive cough, night sweats and chronic sinus inflammation and draining are all but gone. There are a number of other symptoms that may be associated with Moraxella catarrhalis as well and include joint pain/stiffness/inflammation some nerve issues which I also suffer from and ‘perhaps’ are also waning – too soon to be sure.
Moraxella catarrhalis is a fastidious, nonmotile, Gram-negative, aerobic, oxidase-positive diplococcus that can cause infections of the respiratory system, middle ear, eye, central nervous system, and joints of humans. It causes the infection of the host cell by sticking to the host cell using trimeric autotransporter adhesins.
Occurrences in patients with IPF and COPD are noted. In my case, I believe the bacterial infection came first and, perhaps, was a significant contributing factor to my developing PF in the first place and for subsequent exacerbations.
My purpose in writing this is to give you information and make a suggestion… If any of this rings a bell with you I encourage you to get in touch with your care team and push for sputum cultures to check it out.
Moraxella catarrhalis is easily masked/confused for normal flora and therefore not easy to detect. The quality of the sputum sample and the quality of the lab to which it is submitted may affect the results. Three of my sputum samples went to LabCorp and only one came back positive. A fourth was submitted to University of Washington hospital labs and was positive. It is also resistant to some antibiotics and perhaps that explains why earlier prescriptions did not knock it out.
Thanks!
-
After being diagnosed with IPF my Pulmonary Dr. advised me that regular, long term use of albuterol is harmful to the lung tissues. I believe he indicated it could thin/weaken them. I’m using one inhaler, the powdered steroid type (Advair) up to twice per day when I think it could helpful to relieve asthma like symptoms.
-
John Oman
MemberSeptember 19, 2019 at 9:37 pm in reply to: Diet additions that might help AND WEI Institute cure claim – really?@rjshank
Hi Richard. Hope you are doing well. I’m a newbie here and just started looking into WEI. On Feb 1 2019 you indicated that you just started taking their products. I haven’t found any subsequent comments from you regarding how you are doing with it and what you think. If you have, could you point me in the right direction?
-
John Oman
MemberFebruary 9, 2022 at 10:59 am in reply to: Possible Cause of IPF – Ammonia ingestion and Statin?? Progressive?Stuart, Actually I know very little about it and I have more questions than answers. I participate in a large PF support group and I believe there are several in the group who have autoimmune related PF and they’ve been in the group for many years with little or no PF progression. It is my understanding that they take immunity suppressing drug(s) and do not take OFEV or Esbriet (the only FDA approved drugs for treating PF). This is an apparent contradiction to the often stated fact that PF is a progressive, fatal disease. So, maybe they don’t actually have PF? Or, maybe there is some autoimmune cause(s) of PF that yield a more forgiving form of PF? Or, perhaps I’m mistaken about details of the cases I’m referring to. We have another support group session coming up near the end of the month and I’ll try to ask a bit more about it. Thanks! JohnO
-
Toni. I also have IPF, diagnosed 3 years ago. I’m no medical expert, but…
On waking up from your several hour nap, in addition to high BP and HR, are you also breathing rapidly (breathless)? Even if not, I suggest you immediately check your SpO2 level with a pulse oximeter.
Have you been prescribed supplemental oxygen?
Do you have sleep apnea? Have you had a sleep study done?
Hope you find a solution.
JohnO
-
I’ve been using the Inogen TAV with my oxygen tanks for over a year. I find it very useful for my purposes. However, my need and purpose may differ dramatically from yours. I do not use supplemental oxygen except during physical exertion. I classify physical exertion as anything more strenuous than a leisurely walk on flat ground. I do not use it to go shopping (though I do get a store shopping cart and it tends to make walking easier). Nor do I use it climb a single story of stairs.
To walk at normal rate on flat ground (and keep up with wife and kid), I use the TAV at a setting of “1” which I believe is equivalent to about 2 liters per minute (lpm) continuous flow. For a faster (or slightly up hill) cardio walk, I use a setting of “2” which I believe is equivalent to about 4 lpm continuous flow. For walking up grade or climbing multiple stories of stairs, I use a setting of “3” which I believe is equivalent to about 6 lpm continuous.
The TAV comes with a special canula that jets higher pressure O2 through a venturi in each nostril. This tends to pull additional air in along with the O2 and, supposedly assists your inhale by putting a little pressure behind it. Hence the name Tidal Assist Valve (or Venturi?).
What I like most about the TAV: 1) I can put the tank on my back (in a back pack) with the TAV controller unit hanging from a neck pendant on my chest or in a pocket. As my level of exertion and corresponding need for O2 changes, I can simply push the ‘increase’ or ‘decrease’ button without having to stop and access a regulator on top of the tank. 2) It is the most effective, efficient ‘conserving regulator’ on the market (that I know of and I’ve tried quite a few). It provides all of the O2 in a single pulse at the beginning of the inhale. Increasing to the next level increases the duration of the pulse. It does a very good job at stretching the O2 in the tank, a big plus…
As to the Tidal Assist function provided by the special venturi cannula? For me, I do not sense any benefit from it. I also find it a bit fragile and a bit more difficult to fit correctly in the nose. They are also expensive to replace. So I’ve stopped using their special venturi cannula and use a standard cannula instead.
-
John Oman
MemberOctober 21, 2021 at 2:30 pm in reply to: How does taking Prednisone help IPF patientsMark – Is you cough a productive cough? You mention phlegm so I assume it is. Is a portion of the phlegm coughed up in the morning thick/viscous and colored?
-
Hi Mal,
Let me first say I’m not a doctor and do not play one on TV.
Decades ago I was diagnosed with chronic bronchitis with the primary symptoms being chest wheezing, crackling and chronic productive cough. I was told nothing could be done about it and given inhalers to ease symptoms. I also suffered from sinus pressure & drainage, sense of pressure/swelling in ears, forehead, around left eye, stiffness in joints, acne like rash on nose and upper cheeks and back/shoulders. I named it chronic systemic inflammation. CTs, MRIs, nasal endoscopy showed nothing. I floated the idea a number of times over the decades that I might have a bacterial or fungal or ? infection and suggest that sputum/mucus cultures might find something. I was repeatedly told it wasn’t indicated and wouldn’t show anything. I was diagnosed with IPF 2.5 years ago and a about a year after that I was seen by an intern at the clinic and conveyed to him the above chronic systemic inflammation symptoms and suggested a sputum culture. He said sure and wrote up the lab order. Bingo – A bacterial infection, heavy infestation. After a double course of antibiotic, my symptoms improved but I still felt there was something more. Another sputum culture lab order – BINGO – a second/different bacterial infection, heavy infestation. After another double course of a different antibiotic, the chronic system inflammation symptoms I mentioned above all disappeared. My chronic bronchitis like symptoms, the wheezing, crackling and productive cough have become less severe over time. I’m not suggestion you or others have bacterial infections like I did, that’s my story.
Like you, my coughing used to be triggered by lots of things including starting to talk. Now, for the most part, I initiate my coughing intentionally for the purpose of loosening & coughing up sputum. It is my sense/thinking that, over time, I have reduced the amount of sputum buildup that was normally collecting there. Note that I do not claim that my O2/CO2 lung function has improved. However, I am definitely breathing easier, with less effort, and coughing and that results my feeling better and being more interested in engaging in higher levels of physical and social activity.
Of course the sputum keeps getting replaced so you have to keep working at it. How do I work at it?
Note- I cleared the following with my Dr. first! I take bromelain and D-Hist (you can google them) to assist in loosening up sputum. Several times per week I do deep/max inhale and exhale exercise while seated and gentle /easy twisting/stretching. This triggers coughing and you soon figure out what stretches and twists are productive. Any sort of work/exercise with sufficient exertion to get your heart rate up for cardio exercise and use supplemental oxygen to keep your O2 saturation up.
I wish you well and hope that might be able to get the cough more under control.
-
Malcolm,
Is your cough a dry cough? Or a productive cough (do you cough up mucus/sputum that you swallow or spit out)? If it is a productive cough (as mine is), I have a story to tell and a bunch more questions that might be helpful. Thanks!
