Lungs ‘Primed’ for Severe COVID-19 in People With IPF-like Disorders
Written by |
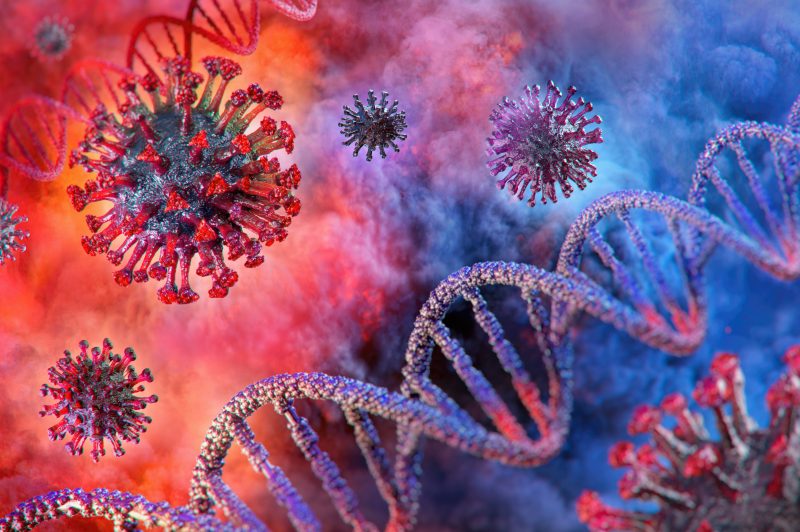
Corona Borealis Studio/Shutterstock
Changes in gene activity and immune cell populations in the lungs of people with chronic lung diseases, such as idiopathic pulmonary fibrosis (IPF), may predispose these patients to severe COVID-19, a study indicated.
“Our results suggest that patients with chronic lung disease are molecularly primed to be more susceptible to infection by SARS-CoV-2,” Nicholas Banovich, PhD, one of the study’s senior authors, said in a press release.
The study, “Chronic lung diseases are associated with gene expression programs favoring SARS-CoV-2 entry and severity,” was published in the journal Nature Communications.
Chronic lung disease is a significant risk factor for hospitalization and death due to SARS-CoV-2 infection — the virus that causes COVID-19.
People with IPF, a chronic lung disease characterized by progressive scarring (fibrosis) and stiffening of lung tissue, are especially vulnerable to severe COVID-19, in which the virus triggers an out-of-control immune response that often leads to ventilation and prolonged hospitalization.
However, the underlying molecular mechanisms responsible for this increased risk are unknown.
An international team of scientists co-led by the Translational Genomics Research Institute in Arizona analyzed 611,398 single cells isolated from the lungs of healthy people (a control group) and those with chronic lung disease to identify molecular changes that may contribute to poorer COVID-19 outcomes.
“It was recognized early in the pandemic that patients with chronic lung diseases were at particularly high risk for severe COVID-19, and our goal was to gain insight into the cellular and molecular changes responsible for this,” said Jonathan Kropski, MD, another of the study’s senior authors.
Cells from IPF patients were examined, along with those from people with chronic obstructive pulmonary disease (COPD) and interstitial lung disease (ILDs) other than IPF.
Researchers used RNA sequencing to measure gene expression in lung epithelial cells — those that line the airways — including AT2 cells. They focused on assessing the expression, or activity, of genes that encode proteins found on the surface of AT2 cells that may facilitate viral entry and infection.
Results showed the two major SARS-CoV-2 cellular entry proteins, ACE2 and TMPRSS2, have similar expression profiles in samples from patients and healthy controls. No major differences were found in other protein factors as well.
However, a viral entry score — calculated based on the average expression levels of all SARS-CoV-2 entry factors — was significantly higher in samples from people with chronic lung diseases.
“Together, these data suggest CLD [chronic lung disease] is associated with modest changes in expression of established SARS-CoV-2 entry factors, and alternative mechanisms are likely additionally responsible for observed differences in outcome severity,” the team wrote.
Researchers next focused on underlying gene expression differences in pathways known to mediate the antiviral response. Many of these genes were significantly altered, including those responsible for restricting viral entry and replication, and serving as essential regulators of the body’s immune response, such as immune signaling proteins (cytokines).
Among all cell types that line the airways, AT2 cells were the ones with the largest number of dysregulated genes in samples from patients compared with controls.
“These data suggest that there are basal differences in the expression profiles of genes regulating viral infection and the immune response in diseased epithelial cells, in particular in AT2 cells and that this epithelial ‘priming’ may contribute to COVID-19 severity and poor outcomes,” the scientists wrote.
Measuring gene expression of the ACE2 receptor in cells isolated from different lung regions found it consistently elevated across all IPF patient sections compared with controls, reaching statistical significance in small airway sections. According to the scientists, these observations indicate “there is a regional concentration of ACE2 [positive] cells within the distal [outer] IPF lung that may promote a more severe localized viral response.”
Furthermore, in all lung sections from IPF patients, there was a significant increase in the expression of a protein called integrin alpha-V beta-6, which plays a key role in fibrosis and is known to activate a gene that suppresses immune responses and increases susceptibility to viral infection.
An analysis of AT2 cells found the expression of ACE2 correlated with the expression of 108 genes from IPF patients, many of which are associated with immune responses.
Recent studies suggest that altered immune regulation, which includes the sustained release of cytokine proteins and excessive inflammation, is linked to severe COVID-19. The team examined immune cell populations taken from lung disease patients, looking for pre-existing immune susceptibility to disease severity and mortality.
Among 12 different immune cell taken from lung disease groups, significant increases were seen in the proportion of CD4 T-cells (helper T-cells), CD8 T-cells (killer T-cells), dendritic cells, and natural killer cells. Compared with controls, all T-cells from patients had higher expression levels of genes associated with cytotoxicity and exhaustion, reflecting a state of T-cell malfunction.
“The genetic changes in immune cells, especially in specialized white blood cells known as T cells, may diminish the patient’s immune response to viral infection and lead to higher risk of severe disease and poor outcomes in patients with chronic lung disease,” said Linh Bui, PhD, one of the study’s first authors.
Finally, in immune dendritic cells and macrophages from lung disease samples, there was reduced expression of the protein AREG, which is increased in COVID-19 patients. This protein is needed to fight viral infections, and known to be involved in wound repair and inflammation resolution.
“Our data suggest that the immune microenvironment at both the molecular and cellular levels in lungs damaged by chronic diseases may promote severe COVID-19,” Bui said.
This study “indicates that CLD is accompanied by changes in cell-type-specific gene expression programs that prime the lung epithelium for and influence the innate and adaptive immune responses to SARS-CoV-2 infection,” the researchers concluded.