-
Tracking IPF Progression
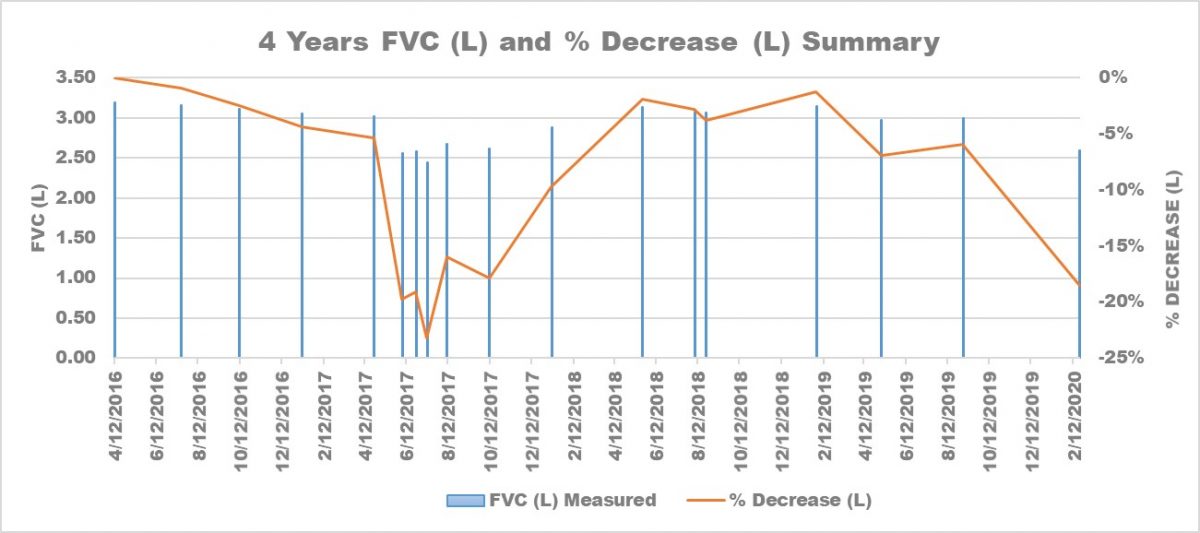 Kevin’s FVC measurements and percentage decrease over four years. (Courtesy of Kevin Olson)
Kevin’s FVC measurements and percentage decrease over four years. (Courtesy of Kevin Olson)On multiple occasions throughout the last 5 years of living with idiopathic pulmonary fibrosis (IPF), I’ve wished for easy and practical ways to track my disease progression. I have explored different apps that help patients track symptoms, easily quantify certain measurements such as pulmonary function tests or manage medications but none ultimately helped me develop a “big picture understanding” of what was going on with my IPF.
As you can imagine, when my co-columnist Kevin Olson shared his experience of tracking his IPF progression in a recent column called, Why I’ve Used Multiple Models to Track My IPF Progression; I was pretty excited to hear from another patient who figured out a way to do this!
Check out Ken’s column which includes a number of different visuals to help readers further understand how he tracked his IPF progression prior to receiving his transplant. I’d also love to hear your thoughts: do you strive to track your IPF progression? If so, what methods or devices work for you and allow you to track the progression of this disease?
Log in to reply.
